Being told you have an ovarian cyst often leaves you with more questions than […]
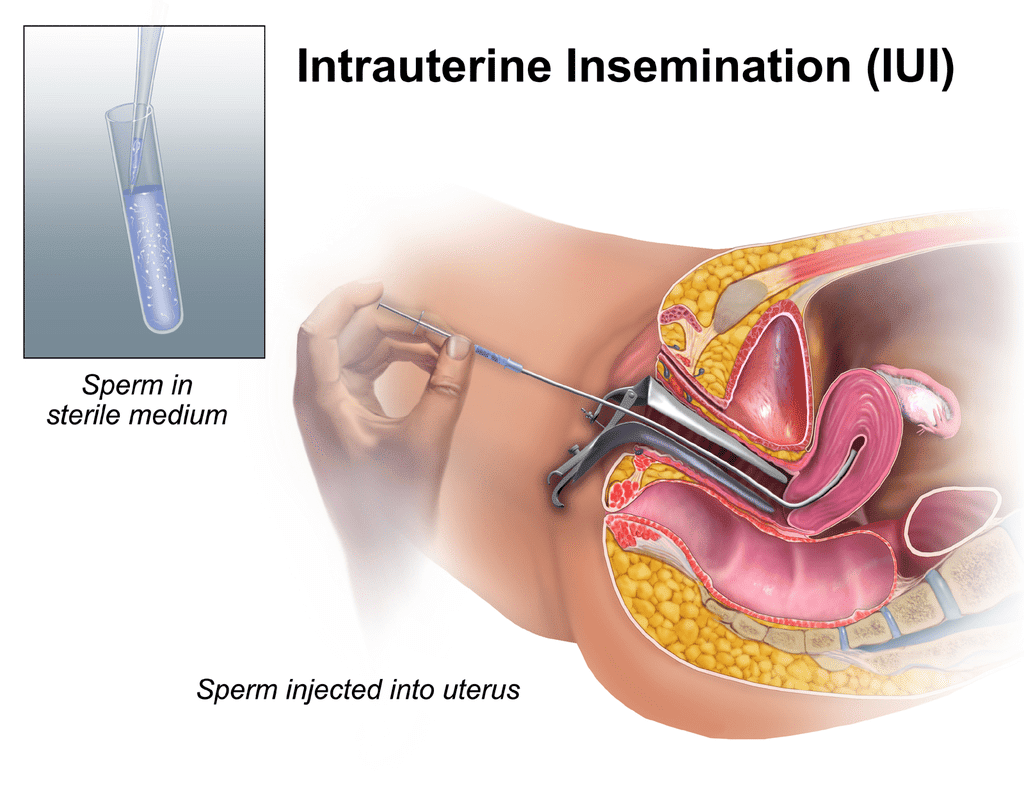
Artificial insemination, or intrauterine insemination (IUI), involves putting washed and concentrated sperm directly inside the uterine cavity around the time that ovulation is expected. This is to increase your chances of fertilisation and pregnancy, and should be done for 3-6 times to maximize your chances of success.
IUI can be recommended in certain situations, including:
You and your partner will be asked to do blood tests to check for communicable diseases such as HIV/syphilis/hepatitis prior.
As IUI requires your fallopian tubes to be in good working order (for the egg to meet the sperm), you will need to do a test for the patency of your tubes prior. This may be in the form of hysterosalpingogram (HSG) or laparoscopy.
The process involves:
IUI is a fast and safe procedure. Risks are low and may include:
Depending on you and your partner’s condition and preferences, your gynaecologist may discuss proceeding on to in-vitro fertilisation (IVF) if you have attempted several rounds of IUI without getting pregnant.
Photo credit: BruceBlaus / Wikimedia Commons
Being told you have an ovarian cyst often leaves you with more questions than […]
Chronic bloating. Lower back pain. Fatigue that lingers even after rest. These are symptoms […]
Many women live with Polycystic Ovary Syndrome (PCOS) without realising fact from fiction. This […]





Aster Gynaecology © | All Rights Reserved.