
An overactive bladder (OAB) is a disorder of the bladder where involuntary contractions of the bladder result in a frequent and urgent need to urinate, causing multiple restroom visits, even throughout the night – a condition known as nocturia. In Singapore, some women with OAB also experience urge incontinence (UI), where they unintentionally leak urine shortly after feeling a strong urge to urinate. This can lead to difficulty reaching the toilet in time when the urge to urinate arises.
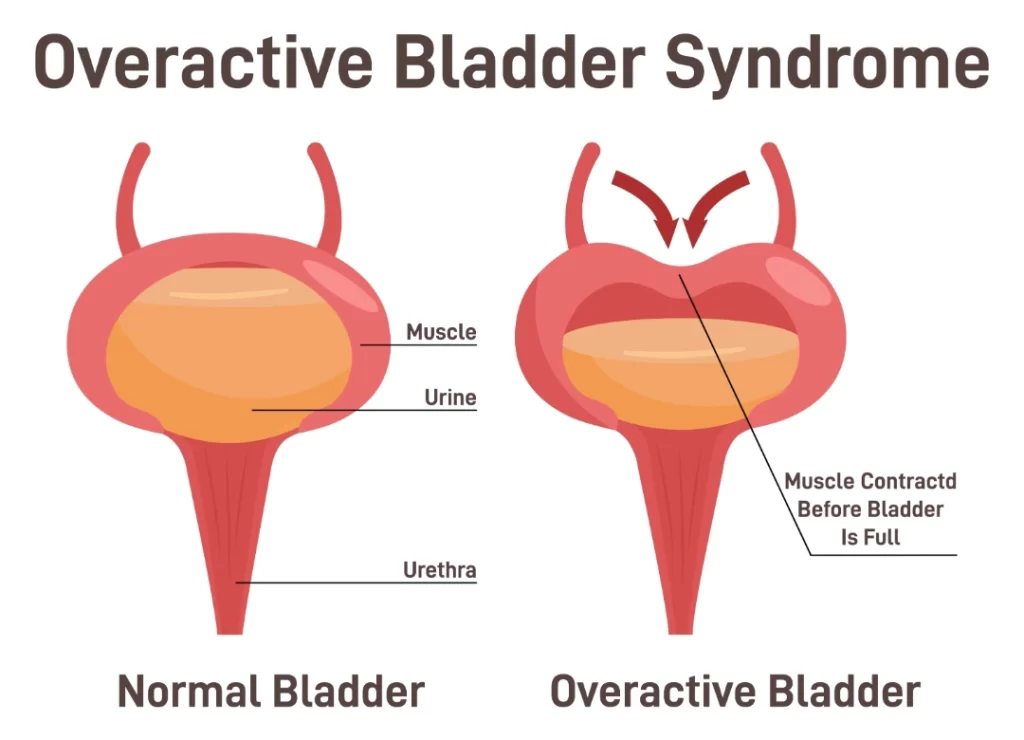
The primary cause of overactive bladder and urge incontinence is the involuntary contraction of bladder muscles attempting to expel urine. This can be temporary, such as when caused by a urinary tract infection (UTI) that eventually clears up. However, persistent cases can result from nerve damage due to factors such as ageing or underlying medical conditions such as diabetes, stroke, or dementia.
Other contributing factors include:
Additionally, weakened pelvic floor muscles may also lead to pelvic organ prolapse (POP), characterised by the descent of the bladder, uterus, or rectum into or beyond the vagina. Consequently, it is common for women to experience both urinary incontinence and some degree of POP.
The symptoms of an overactive bladder include:

Overactive bladder itself is not usually painful, but it can cause discomfort and inconvenience due to the frequent and urgent need to urinate. The sensation of urgency and the frequent trips to the bathroom may disrupt your daily activities and quality of life. However, the condition is primarily characterised by the sudden and strong urge to urinate. If you are experiencing pain along with these symptoms, it could indicate another underlying issue that needs to be addressed. While not inherently painful, an overactive bladder can impact your comfort and daily routine.
In Singapore, various factors can increase the risk of developing an overactive bladder; these are:
If you suspect you have an overactive bladder, your doctor will conduct a thorough evaluation to make a diagnosis.
After going through your medical history, the following tests may be performed:
You may not be fully cured of this persistent condition, but there are effective methods to manage your symptoms and prevent them from dominating your daily life.
The main form of treatment for an overactive bladder involves making lifestyle changes, which can often lead to significant improvement in symptoms. Conservative treatment options for an overactive bladder include:

If lifestyle changes show insignificant results, medications are often prescribed alongside the aforementioned modifications. These drugs relax bladder muscles, allowing for longer intervals between urination. It is important to note that these medications require several months before results are noticeable.
Side effects may include dry eyes, mouth, skin, and constipation. Finding the right medication may require experimentation, and certain medical conditions may limit their suitability.
In more severe cases, secondary options involve more invasive procedures. These include Botox injections directly into your bladder (administered through a scope under local or general anaesthesia) and nerve stimulation (percutaneous tibial nerve stimulation). These methods may need to be repeated every six months due to their temporary effects.
What tests do I need to diagnose OAB?
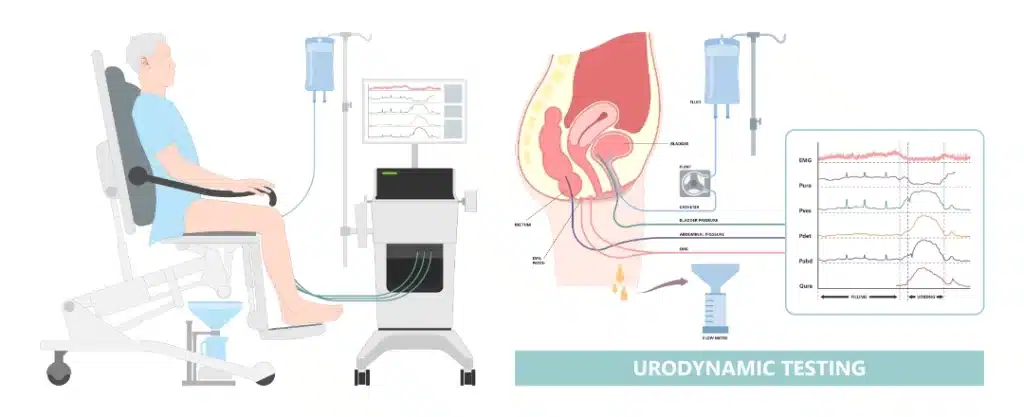
It is crucial to consult with a urogynecologist, a specialist concerning female urinary issues to determine a correct diagnosis and to discuss available treatment options. During this consultation, your medical history will be reviewed, and a pelvic examination will be conducted to assess the presence of any pelvic organ prolapse and the condition of your pelvic floor muscles. Further evaluations may be suggested based on your symptoms, such as ultrasound scans to examine your uterus and ovaries, urine tests, bladder scans to measure the residual urine post-void, and potentially a urodynamic study to assess your bladder function and muscle stability.
Can an overactive bladder be cured?
An overactive bladder cannot go away on its own. Treatment for an overactive bladder is necessary to prevent symptoms from worsening. Make an appointment with us today and get treated for your overactive bladder.