In a ground-breaking White Paper on Women’s Development released on 28th March 2022, the Singapore government has announced that women aged 21 to 35 will soon be able to opt for social egg freezing in Singapore regardless of their marital status.
This is a huge (and exciting!) change from existing criteria, where only women who are undergoing treatment known to affect fertility are allowed to undergo egg freezing i.e. for medical reasons.
Egg freezing is where eggs harvested from your ovaries are frozen and kept for later use. It is important to note that the younger you are at the point of egg freezing, the higher the chance of good response to ovarian stimulation and obtaining good quality eggs for storage. Good quality eggs have a higher chance of forming good quality embryos that then lead to successful pregnancies subsequently. This is different from embryo freezing, where eggs are fertilised with sperm to form embryos first before freezing.
Currently, egg freezing in Singapore is most commonly done when a woman in her reproductive age who desires children in the future is diagnosed with cancer and needs to undergo treatment e.g. chemo or radiotherapy which can potentially affect her future fertility.
Egg freezing in these scenarios (before she starts fertility-affecting treatment) can help preserve her fertility and potentially allow her to have her own children after recovering from cancer.
However, women facing these scenarios may not have the awareness of this option, the mental preparedness in deliberating about future children in the face of a new cancer diagnosis, and/or the luxury of time to defer cancer treatment (as egg freezing requires some preparation work).
Those who do wish to consider medical egg freezing in these scenarios typically need to undergo:
In other cases, egg freezing is done for social reasons i.e. a woman who is advancing in age and desires children in the future but has not found a suitable life partner yet.
This is because women are born with a finite number of eggs and the number and quality of these eggs decline with age. This process of “elective” or “social” egg freezing is not allowed in certain countries – until recently, Singapore was one of them, forcing many women in such situations to travel overseas for this purpose.
As of early 2023 though, women aged 21-35 will be allowed to undergo social egg freezing in Singapore, with the introduction of the Assisted Reproduction Services Regulations under the Healthcare Services Act.
They will however be required to undergo counseling to make sure that they understand the risks, success rate, costs and invasive nature of egg freezing before going ahead with the procedure. This marks a drastic change from Singapore’s typical conservative approach, and may pave the way to allowing older women to have children later on in life – something that was not possible previously.
To ensure you are in good health to undergo the process of egg freezing and to be a potential parent in the future).
To check for conditions that may affect your fertility.
This typically includes blood tests for anti-mullerian hormone (AMH) and follicle stimulating hormone (FSH), as well as ultrasound scan for antral follicle count (AFC).
e.g. HIV/Syphilis/Hepatitis
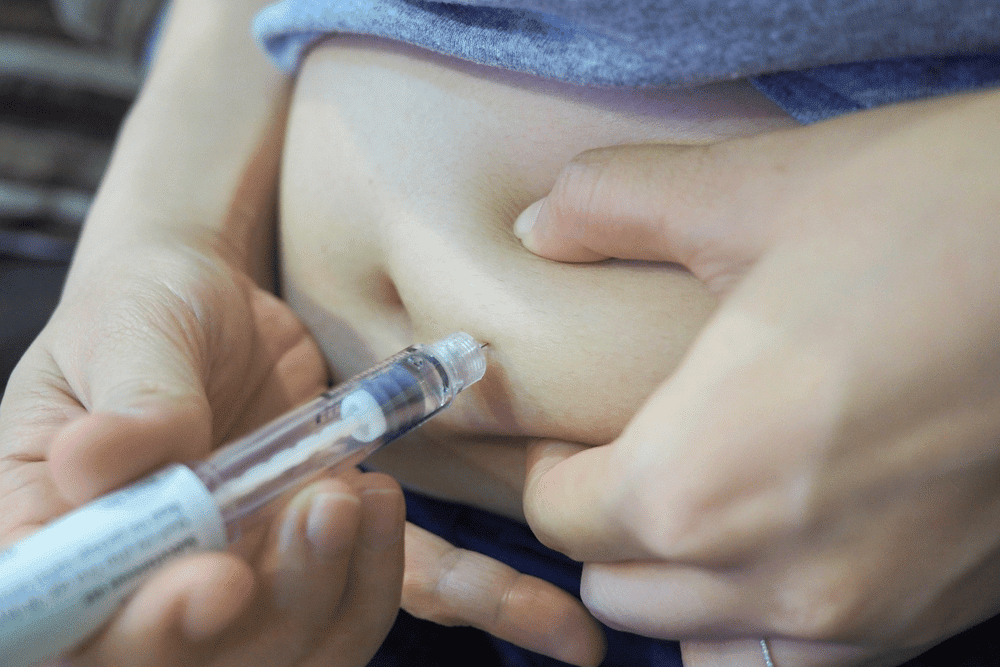
Ovarian stimulation
This involves hormone injections (self-administered at home) to stimulate the development of more than 1 egg at the same time. Further injections are required to prevent premature ovulation, and to help with maturation of the eggs.
Ovarian monitoring
This involves regular ultrasound scans to monitor follicle growth and blood tests to measure your hormone levels – this allows your gynaecologist to adjust your injection doses according to your response.
Egg collection (oocyte retrieval) and freezing
This is usually done as a day surgery under general anaesthesia. A fine needle is inserted through your vagina under ultrasound guidance to tap on your follicles for egg collection. This takes 15-30 minutes. These eggs will be checked for quality and maturity, and suitable ones selected for freezing. The most common method is vitrification, where cyroprotectants are used to prevent formation of ice crystals during rapid cooling. This ensures a higher survival rate of the eggs when thawing later on.
Storage of frozen eggs
Your eggs are kept frozen in the laboratory until the time you need to use them.
After vitrification, the frozen eggs are kept in the laboratory in tanks of liquid nitrogen. Once you are ready to use them, the eggs will then be thawed and injected with sperm to form embryos, which will be transferred into your womb (uterus).
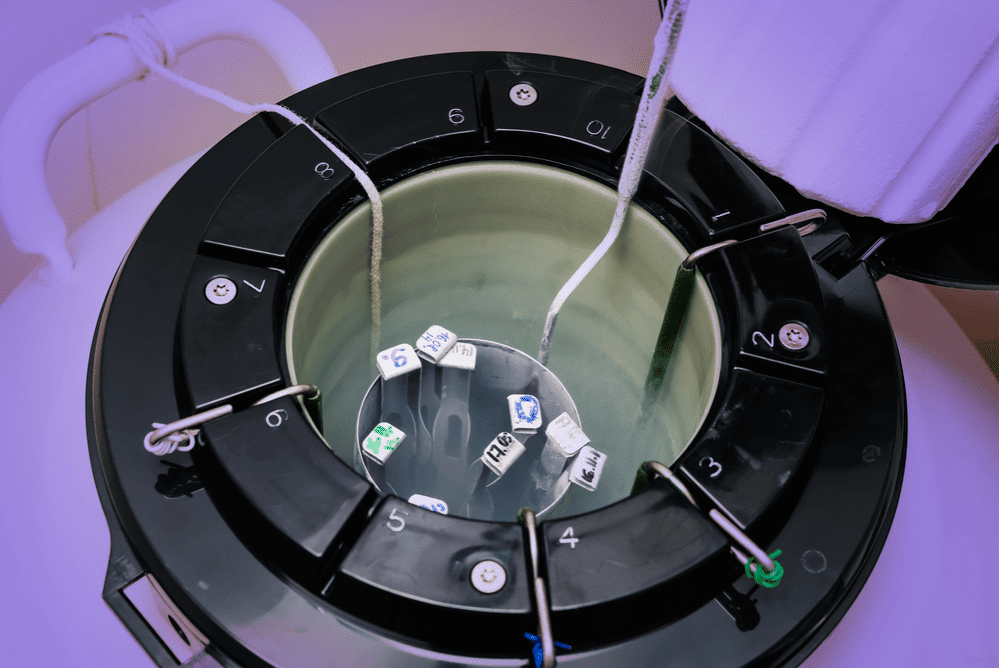
There is technically no limit as to how long the eggs can be kept frozen for, as unlike in the body where advancing age results in poorer quality and few quantities of eggs, the frozen eggs have essentially been “frozen in time”.
Although there are no official records yet on the oldest frozen egg that has successfully resulted in a pregnancy, the oldest frozen embryo known to result in a baby is 27 years old1. This gives you an idea of how far along freezing techniques have come all these years!
There will also be several decisions you need to make for your frozen eggs, namely:
You will also need to understand that in order to conceive with frozen eggs, you will need to undergo the rest of the in-vitro fertilisation (IVF) process when you are ready to use your (thawed) eggs.
As the process of egg freezing involves ovarian stimulation, there can be potential risks to women undergoing this. One risk is ovarian hyperstimulation syndrome (OHSS).
Most women usually end up with mild OHSS, but some may experience severe OHSS that may be potentially life-threatening. Symptoms of OHSS include:
In severe cases of OHSS, you may require hospitalisation and treatment.
Oocyte retrieval is performed under general anaesthesia, risks include side effects from anaesthesia, and procedural risks include pain, pelvic infection, injury to surrounding organs such as bowel, bladder or major blood vessels.
These risks are typically low as oocyte retrieval is performed under continuous ultrasound guidance by trained specialists.
There were previous concerns over theoretical risks of cancer development later in life from undergoing assisted reproductive techniques (ART); thankfully recent studies have not demonstrated this.
However, it has been shown in a recent Lancet2 publication that babies conceived from ART do have an increased risk of birth defects, and this risk is partly attributable to infertility itself, certain ovulation induction regimen and multiple pregnancies induced by ART.
Ultimately, the major risk of egg freezing is that it may not result in a successful livebirth in future.
Unfortunately, having frozen eggs in storage does not necessarily guarantee your success for pregnancy and livebirth in the future. According to a report released by the Human Fertilisation and Embryology Authority3, women aged 35 years and below who froze their eggs had a 15% successful thaw cycle versus 12.5% for those who froze their eggs aged 40-42.
In terms of a birth, for eggs frozen under 35, there was a 27% chance of a birth compared to just 13% for eggs frozen over age 35. This is the reason why Singapore has restricted social egg freezing to women aged 21-35 years old.
You should know that there is a “drop-out” rate at every stage of IVF – not every frozen egg will survive the thawing process, not every thawed egg will successfully form an embryo after fertilisation with a sperm, and not every embryo that is transferred into the uterus (womb) will result in a successful pregnancy and livebirth.
Even if you do conceive successfully with your frozen egg, it is important to note that older mothers face an increased risk of pregnancy complications overall.
The cost of egg freezing does not differ between medical and social reasons – it can cost $10,000 and above for 1 cycle. The cost will vary depending on the dose of ovarian stimulation drugs – think of it as an expensive lottery ticket – you will need to do prior financial planning before embarking on this journey.
Aside from the financial cost, there will be emotional and mental “costs” to egg freezing as well; not everyone will end up having many good quality eggs at the end of the process for freezing, as the response of each individual woman will vary.
You may have to be prepared to undergo at least a few cycles of egg freezing to ensure that sufficient mature eggs are obtained for freezing to give you a reasonable chance of success.
Also, at the end of the day, you may ultimately end up not using your frozen eggs as circumstances may change.
The rates of frozen embryos resulting in successful pregnancy is higher than that of frozen eggs – simply because:
In other words, you will need to start off with a higher number of frozen eggs compared to frozen embryos to have the same chance of a successful pregnancy.
From a non-statistical point of view however, egg freezing can be better for women as it offers more autonomy. As the process of egg freezing does not require sperm, this becomes an empowering, viable reproductive option for single women who do not have a partner.
Freezing eggs rather than embryos can also help avoid dicey situations when couples split subsequently, with differing opinions on what to be done with the frozen embryos.
There are still gaps even with the latest move by the Singapore government though, as only legally married couples will be able to tap on their frozen eggs for reproduction. This means that women looking to set up a single-parent household with their frozen eggs will still face difficulty doing it in Singapore – for now.
Ultimately, the choice is yours, and the procedure that is best for you depends on what your current life situation is and what your ultimate goals are.
This article was updated on 22 April 2022 by Dr. Ng Kai Lyn.
What is time-lapse monitoring, and what is its benefit?
During embryo development in the lab, embryologists must check the embryos’ progress and quality before picking the best ones to be transferred back into the uterus. The best embryo environment needs to be stable, with fixed temperatures, oxygen level and a good culture medium. Checking the embryos, however, involves handling the embryo in and out of the incubator daily. Time-lapse monitoring, where regular images are taken of the embryos to record their development, allow embryologists to monitor the embryos without having to remove them from the incubator. This new technology is believed to aid the best embryo selection for IVF.
Is time-lapse monitoring routine for IVF?
No. Time-lapse monitoring is not routine for IVF cycles and facilities are not available at all IVF labs. Your gynaecologist will be able to discuss further with you regarding this technology and if it is advisable in your case.
What is the difference between Pre-implantation Genetic Diagnosis (PGD) and Pre-Implantation Screening (PGS)?
These are both pre-implantation genetics tests (PGT) done on the embryo before embryo transfer. The embryos are obtained through a process called in-vitro fertilisation (IVF).
| PGS | PGD | |
| Testing for normal chromosome numbers (23 pairs) | What it involves | Test for specific, known genetic disorder |
| 1 or more cells are taken from embryo while it is still in the lab | How it is done | 1 or more cells are taken from embryo while it is still in the lab |
| To increase IVF success and reduce miscarriages | What its purpose is | To reduce risk of passing on the specific genetic disorder |
| Couples with recurrent miscarriage, low quality eggs, multiple failed IVF cycles | Who it is recommended for | 1 or both parent are carriers of known genetic disorder |
Depending on the country, PGD and PGS are governed by different rules and regulations. You should discuss with your gynaecologist to see if you are suitable for, or require pre-implantation genetic tests.
OHSS is a potentially serious complication from fertility treatment, where there is an excessive response to ovarian stimulation medications during in-vitro fertilisation (IVF). Rarely, this can occur after ovulation induction.
OHSS can be classified as mild, moderate or severe. Mild OHSS is common, occurring in 33 in 100 women undergoing IVF, while moderate/severe OHSS is rare, occurring in 1 in 100.
Ovaries go into overdrive from ovarian stimulation medications, become larger and release chemicals into the bloodstream. This causes your blood vessels to be leaky and fluid leaks out into your abdomen, lungs and sometimes around the heart. Other organs that may be affected include the kidney and liver. Blood clots and rarely, death have been associated with OHSS.
Symptoms include:
Majority of symptoms will go away in about a week’s time (or whenever your periods come if your IVF was unsuccessful). However, if you fall pregnant from your IVF, your symptoms will last a few weeks or longer. Pregnancies complicated by OHSS may be at a higher risk of having pre-eclampsia or preterm delivery, but the baby will not be affected.
If you suspect you may be developing OHSS, you should contact your gynaecologist immediately.
Your gynaecologist will take a detailed medical history and perform a physical examination. Your temperature, blood pressure, pulse rate, oxygen levels, weight, waistline, intake and output (urine volume) will be measured. You will be allowed to eat and drink to thirst. An ultrasound scan will be performed to check the size of your ovaries and the amount of fluid in your abdomen. If necessary, additional scans may be ordered to check for other complications such as fluid in your lungs, around your heart or any blood clots in your legs or lungs. You will need blood tests to check how concentrated your blood is as well as your liver/kidney function.
Things you will need whilst in hospital may include:
Most OHSS will get better with time, close monitoring and supportive treatment.
ICSI is when a single healthy sperm is injected into a good quality egg.
There are some reasons why ICSI may be recommended including:
No. This is because there are several problems that can still occur along the way:
The risk of having a birth defect with ICSI is similar to IVF but slightly higher than if you were to get pregnant naturally. If you got pregnant naturally, the risk of a major birth defect is 2-3%.
The risk of birth defects with ICSI is thought to be related to infertility and not ICSI itself.
You will have been contacted for an embryo transfer. Prior to the transfer, your gynaecologist will discuss with you the number of embryos for transfer and if there are any remaining ones for freezing.
Embryo transfer does not usually require anaesthesia. You will be asked to have a full bladder so that the uterus will be better seen on a trans-abdominal ultrasound. The procedure lasts for 5-10 minutes. You will be positioned similar to doing a Pap smear, and a trans-abdominal scan done to visualise your uterus. A speculum will be inserted in your vagina, and your cervix cleaned. The embryologist will verify your identity and your embryos. A thin soft tube containing your embryos will be inserted into your uterus through your cervix and placed into your uterus (this will be seen on ultrasound as well).
You will be asked to rest for 30 minutes or so after the transfer. You can eat and drink as per normal. You will be allowed to go home and should be able to return to your usual activities the next day, although medical leave for rest will usually be given.
You will be given an appointment to return for a blood test to measure your pregnancy hormone levels in about 2 weeks. You will need to continue on your hormone medications (progesterone support).
The risks are very low and may include mild temporary lower abdominal cramps or spotting.
Some tips:
Do contact your gynaecologist if you experience fever, abdominal pains or heavy vaginal bleeding.
Most importantly, rest, relax, take it slow, seek support from your partner and hope for the best!
Embryo freezing (EF) is where embryos obtained from in-vitro fertilisation (IVF) are frozen and kept for later use. This is different from egg freezing, where eggs harvested from ovaries are directly frozen (without fertilisation from sperm) and kept for later use.
EF is most commonly done when surplus embryos are produced from an IVF cycles and only 1-2 embryos are being transferred back into the uterus. EF allows a woman to have a future chance of pregnancy if her initial embryo transfer is unsuccessful – without having to go through the whole IVF cycle again. You can read more about the process of IVF here.
Another common reason is “freeze-all”. This is where a woman needs time to recover from her egg collection e.g. high risk of developing ovarian hyperstimulation syndrome (OHSS). Freezing all embryos and allowing her time to recover means a frozen embryo transfer will be planned at a later date.
Another reason why EF is done is when a women in her reproductive age desiring children is diagnosed with cancer and need to undergo treatment e.g. chemo- or radiotherapy which potentially affects her future fertility. EF in this case can preserve her fertility and allow her to have her own children with her partner after recovering from cancer.
The most common method of EF is vitrification, where cryoprotectants are used to prevent formation of ice crystals during rapid cooling.
Studies have shown that the freezing and thawing process, and the duration of storage does not affect the babies which result from these frozen embryos. Pregnancy rates from frozen embryo transfers may in fact be better in certain cases.
About 85% of embryos survive the thawing process.
Read more about social egg freezing in Singapore here.
You will be scheduled for egg collection approximately 36 hours after your injection to trigger egg maturation. You will be asked to fast before the procedure.
Egg collection is usually done under general anaesthesia as a day surgery procedure. It lasts for 15-30 minutes. You will be positioned similar to doing a Pap smear, and a transvaginal ultrasound performed to locate your follicles. A fine needle will be inserted through the vagina to tap the follicles and retrieve your eggs. These will be sent to the lab where they will determine the number of eggs collected and the egg quality.
After you wake from anaesthesia, you will be allowed to eat and drink. Your temperature, blood pressure and pulse rate will be monitored. You will be allowed to go home with someone accompanying you (as you cannot drive). You should be able to return to your usual activities the next day, although medical leave for rest will usually be given.
On the same day, your partner will be asked to produce a semen sample for the lab, where it will be processed and good quality, healthy sperm picked out.
You will receive information about the number of eggs, maturity and quality of eggs after the procedure, as well as the embryo development process and when to return for an embryo transfer.
Hormone medications (progesterone support) will be prescribed – this prepares the lining of your uterus to receive the embryos.
The risks are low as the procedure is done under continuous ultrasound guidance, but can include:
It is normal to experience mild cramping and vaginal spotting for a few days after the procedure. Some tips:
Do contact your gynaecologist if you experience fever, abdominal pains or heavy vaginal bleeding.
Most importantly, rest, relax, take it slow, seek support from your partner and hope for the best!
What is assisted hatching?
This is an additional procedure that some couples undergoing in-vitro fertilisation (IVF) may require. Embryos are surrounded by a hard “shell” which is made up of an outer layer of cells – this is called the zona pellucida.
To implant into the uterine lining, embryos must “hatch” i.e. break free of this shell. Assisted hatching helps the embryo by using laser in the lab to make a small crack in their shell so that they can implant more easily. This can be done for both fresh and frozen embryos.
Is assisted hatching required for all?
No. Assisted hatching may be helpful in women who have failed previous IVF cycles. Occasionally, this may be done for embryos that require pre-implantation genetic tests.
Does assisted hatching pose any risk to the embryo?
There is a slightly increased risk of identical twins. Embryos are very rarely damaged from the process of assisted hatching.

Aster Gynaecology © | All Rights Reserved.