Being told you have an ovarian cyst often leaves you with more questions than […]
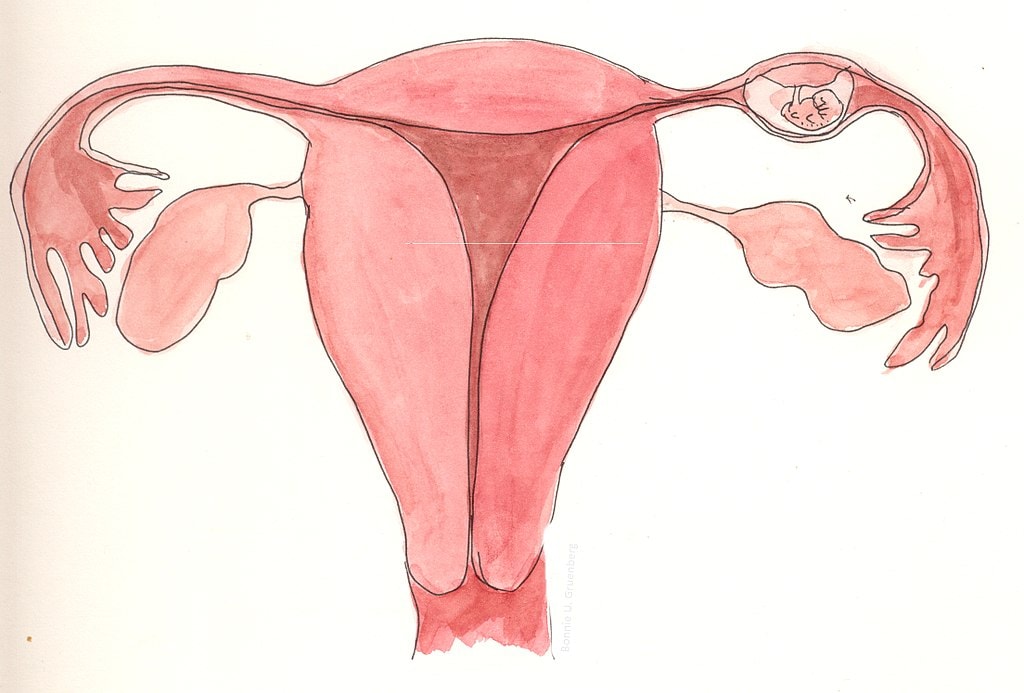
An ectopic pregnancy is a pregnancy that occurs outside the uterus, most commonly in the fallopian tubes (90%). Rarely it can occur in the ovary, cervix or at the site of a previous caesarean section scar. An ectopic pregnancy is not a normal pregnancy and cannot be turned into one, as the only place that can sustain a pregnancy to term is the uterus.
1 in 50 pregnancies turn out to be ectopic pregnancies. Once you have had a history of an ectopic pregnancy, you will have a higher risk (10-15%) of having another ectopic pregnancy in the future.
Some women may have no symptoms. Some women may have mild lower abdominal pain or discomfort, or some vaginal bleeding.
The dangerous thing about an ectopic pregnancy is that it can rupture and cause massive, life-threatening internal bleeding. In the event of a ruptured ectopic pregnancy, one needs to be rushed to the Emergency Department as one may experience severe abdominal pain, shoulder-tip pain, giddiness/dizziness, vomiting, fainting or even collapse.
If you suspect that you may have an ectopic pregnancy, you should see your gynaecologist immediately.
Your gynaecologist will need to take a detailed menstrual history and perform an abdominal and pelvic examination to look for any tenderness. A transvaginal ultrasound will be done to look for the location of the pregnancy. If your uterus looks empty on the scan, it may be too early for your pregnancy to be seen on ultrasound scan and you will need to take a blood test to measure your pregnancy hormone (b-hcg). Depending on the b-hcg levels, you may need to have your b-hcg trended every 48 hours, with an ultrasound repeated to ascertain the diagnosis of an ectopic pregnancy. Until then, you will need to stay vigilant and watch for any symptoms that may suggest ruptured ectopic pregnancy (see above).
This depends on your symptoms, blood pressure, pulse rate, b-hcg levels, size of ectopic pregnancy and willingness for regular follow-up. There are 2 main options:
1. Methotrexate (MTX) injection
This is an intramuscular injection which stops division of pregnancy cells. It is also used in chemotherapy, but the dose given for an ectopic pregnancy is much lower. The ectopic pregnancy cells shrink and are absorbed by your body. The success rate is 90% (lower if your b-hcg level is higher). 15% of women may need a 2nd injection if their response to the 1st injection was insufficient. You will be required to return regularly to trend your b-hcg levels. You will need to stay vigilant and watch for any symptoms that may suggest ruptured ectopic pregnancy as it can still happen anytime until your b-hcg goes back to normal – this may take 4 to 6 weeks.
You are suitable for MTX if you are stable with no severe abdominal pain or bleeding, your b-hcg is <5000IU, your ectopic pregnancy measures less than 3.5cm on ultrasound scan with no evidence of internal bleeding, there is no fetal heartbeat seen and you are willing to return for regular monitoring blood tests. You should not have kidney, lung, liver or blood disease, be breastfeeding or have an active infection.
MTX is generally tolerated well. Common side effects include pain at injection site, mild lower abdominal discomfort, mild vaginal bleeding. You should not get pregnant for 3 months after MTX injection as it will take some time for MTX to be cleared.
2. Surgery
This is usually done laparoscopically (keyhole). The best surgery to treat an ectopic pregnancy is a salpingectomy(removal of ectopic pregnancy with fallopian tube). This is because the fallopian tube is usually damaged resulting in the formation of the ectopic pregnancy in the first place, and further damaged following implantation of the ectopic pregnancy there.
In very few select patients where their other tube is also damaged, a salpingostomy can be done. This involves making a cut on the affected fallopian tube and removing as much of the ectopic pregnancy as possible. Weekly b-hcg blood tests will be required due to risk of persistent ectopic pregnancy tissue, which may need further treatment. Leaving a damaged fallopian tube behind means you will be at a higher risk of having another ectopic pregnancy (on the same side) in future.
Photo credit: © Bonnie Urquhart Gruenberg / Wikimedia Commons
Being told you have an ovarian cyst often leaves you with more questions than […]
Chronic bloating. Lower back pain. Fatigue that lingers even after rest. These are symptoms […]
Many women live with Polycystic Ovary Syndrome (PCOS) without realising fact from fiction. This […]





Aster Gynaecology © | All Rights Reserved.