Being told you have an ovarian cyst often leaves you with more questions than […]
This is a condition where the lining of the uterus becomes too thick. Although it is not cancer, it can progress to cancer of the uterus in some cases if left untreated.
The lining of the uterus responds to female hormones. Estrogen is involved in the first half of the cycle, where the lining grows and thickens. After an egg is released (ovulation), progesterone comes in to prepare the lining of the uterus for pregnancy. If fertilisation does not occur, the lining is shed and a new cycle begins.
Endometrial hyperplasia occurs when there is excess estrogen without progesterone. This happens when ovulation does not occur and progesterone does not come in. The lining of the uterus continues to grow, the cells of the lining start to crowd together and there is no shedding. If this continues, it may eventually lead to cancer.
Abnormal bleeding is usually the first sign of endometrial hyperplasia. These include:
Your gynaecologist will advise you on the type of endometrial hyperplasia you have, including:
Atypia increases the risk of progressing to cancer.
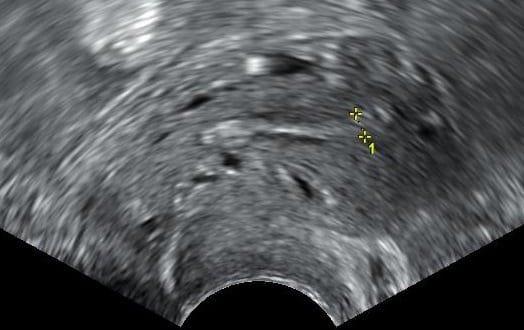
A transvaginal pelvic ultrasound scan is useful to measure thickness of the lining of the uterus; however, the only way to confirm would be through a biopsy of the uterus lining. This is either done in the clinic (endometrial pipelle), or as a day surgery under general anaesthesia (hysteroscopy dilation and curettage (D&C)). The biopsy will need to be examined under a microscope to diagnose endometrial hyperplasia, and whether atypia is present.
This depends on your age, medical conditions, fertility plans, type of hyperplasia and willingness for long-term follow-up. Options include:
Photo Credit: Mikael Häggström / Wikimedia Commons
Being told you have an ovarian cyst often leaves you with more questions than […]
Chronic bloating. Lower back pain. Fatigue that lingers even after rest. These are symptoms […]
Many women live with Polycystic Ovary Syndrome (PCOS) without realising fact from fiction. This […]





Aster Gynaecology © | All Rights Reserved.