Being told you have an ovarian cyst often leaves you with more questions than […]

Many women live with Polycystic Ovary Syndrome (PCOS) without realising fact from fiction. This common condition affects up to 1 in 10 women of reproductive age [1], yet it remains widely misunderstood. This is a major concern as misinformation can delay diagnosis, discourage treatment, and leave many women feeling confused or alone.
PCOS is a hormonal imbalance that can interfere with ovulation, menstrual cycles, and various metabolic processes. Because symptoms vary, and often mimic other conditions, PCOS is frequently misrepresented, especially online.
In this quick read, we’ll clear up some of the most common misconceptions surrounding PCOS, so you can better understand your body, and take charge of your reproductive, and overall health.

Fact: Many women with PCOS do conceive naturally or with support.
It is true that PCOS can disrupt ovulation, which may make conception more difficult. However, it does not mean you are infertile. In fact, many women with PCOS go on to have successful pregnancies.
Ovulation may be irregular or less frequent, but it often still occurs. Identifying ovulatory cycles and receiving timely medical guidance can significantly improve the chances of conception. Fertility treatments, such as ovulation induction, intrauterine insemination (IUI), and IVF, are also effective options for many.
Comprehensive fertility evaluations and tailor-made treatment plans to support women with PCOS on their journey to motherhood can be helpful – this often begins with a thorough evaluation to understand period and hormonal patterns, ovulation cycles, as well as any underlying metabolic issues.
From there, treatment plans can be tailored to each individual’s needs — ranging from simple lifestyle adjustments, and ovulation tracking to medical interventions like ovulation induction, intrauterine insemination (IUI) or in vitro fertilisation (IVF). With the right guidance, and care, many women with PCOS can conceive and have successful, healthy pregnancies.
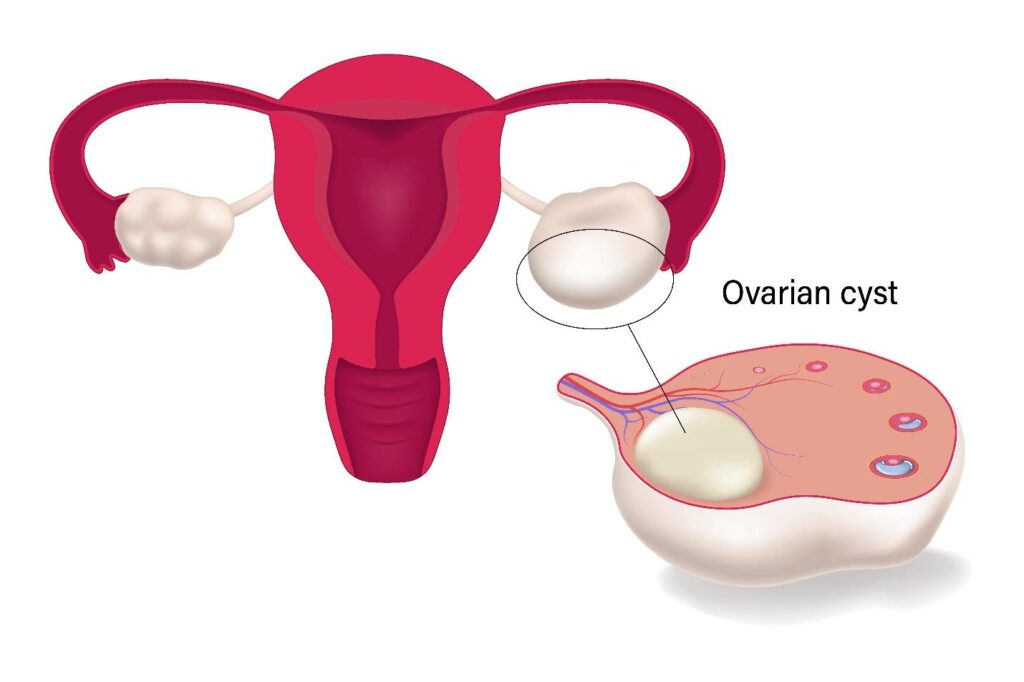
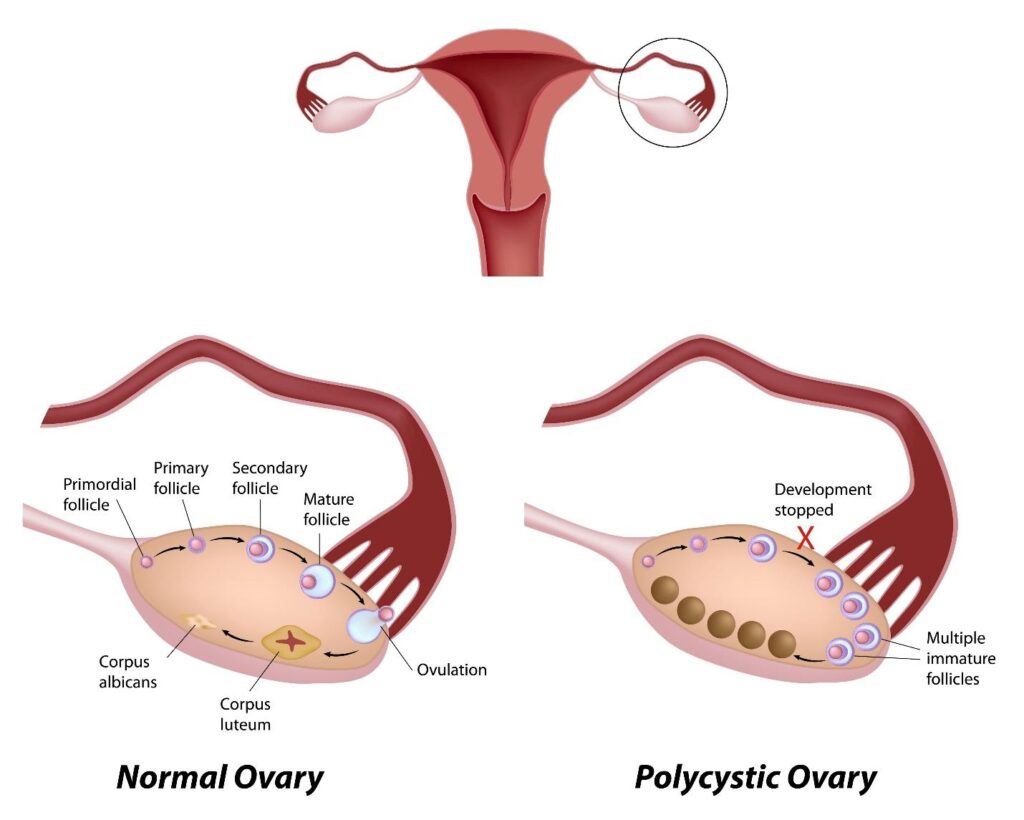
Fact: Not every woman with PCOS has ovarian cysts.
The term “polycystic” can be misleading. It refers to the appearance of the ovaries on ultrasound, which may show multiple small follicles. However, the presence of these follicles, which are often interchangeably called cysts, is just one of the diagnostic criteria.
PCOS is diagnosed based on the Rotterdam criteria, which requires at least two of the following three:
So, it is entirely possible to have PCOS without any visible cysts.

Fact: PCOS is primarily influenced by genetics and hormonal factors.
While lifestyle choices can influence the severity of PCOS symptoms, they are not the root cause. Many women with a healthy lifestyle still develop PCOS due to underlying hormonal imbalances [2], and genetic predispositions [3].
That said, managing weight, eating a balanced diet, and exercising regularly can help regulate insulin levels, and improve hormonal function. But it is essential to approach PCOS management with compassion, understanding, and not blame.
It goes without saying that holistic support plays a vital role in helping women manage PCOS effectively — fostering confidence, resilience, and long-term wellbeing without guilt or shame. With the right information, encouragement, and medical care, women can feel empowered to take control of their health, and navigate their PCOS journey with clarity, and confidence.

Fact: Women of all shapes, and sizes can have PCOS.
Although weight gain, and difficulty losing weight are common in PCOS, the condition also affects women who are lean. Known as “lean PCOS,” [4] this subset often goes undiagnosed because the absence of weight issues can mask underlying hormonal imbalances.
Symptoms like irregular periods, acne or infertility can still occur regardless of body weight. Therefore, body mass index (BMI) alone should never be the basis for diagnosis or dismissal of concerns.
Weight alone should never be used to confirm, or rule out, a diagnosis of PCOS. A thorough assessment of symptoms, hormone levels, and ovarian morphology on scan is essential for accurate diagnosis, and appropriate care.

Fact: PCOS presents with a wide range of symptoms.
While irregular or absent periods are a hallmark sign of PCOS, many other symptoms may indicate hormonal imbalance. These include:
If you are experiencing any combination of these symptoms, it is important not to dismiss them. PCOS can present in many ways, and early evaluation is key to understanding what is going on in your body. Consulting your gynaecologist can help uncover the root cause, and guide you towards effective management.
Remember, timely diagnosis can make a significant difference in preventing long-term complications, and improving overall well-being.

Fact: The pill can manage symptoms, but it is not a cure.
Hormonal birth control is often prescribed to regulate periods, reduce acne, and manage excessive hair growth. However, these effects are temporary, and stop when the medication is discontinued.
PCOS is a long-term condition requiring sustained management. In addition to hormonal treatment, lifestyle changes, supplements, and targeted medications (such as metformin) may be recommended based on your symptoms, and goals.
Managing PCOS effectively often requires more than just medication. A multidisciplinary approach, one that combines medical care with nutritional guidance, metabolic assessments, and lifestyle support, can make a meaningful difference.
Addressing PCOS from multiple angles helps regulate hormones, improve insulin sensitivity, and reduce long-term health risks. By focusing on the whole person rather than just isolated symptoms, women can achieve more sustainable improvements in both reproductive, and general health.

Fact: PCOS has wide-ranging effects on your overall health.
PCOS extends beyond fertility concerns. It is linked to several long-term health risks, including:
This makes regular monitoring, and preventive care essential. Holistic management of PCOS goes beyond addressing symptoms. It involves consistent follow-ups, lifestyle adjustments, and routine health screenings to track hormonal, metabolic, and emotional wellbeing over time.

Knowledge is the first step towards empowerment. If you suspect you may have PCOS, or if you have been diagnosed but feel unsupported, know that you are not alone.
Here is how you can take control:
[1] Ling-Hui Zeng, Rana, S., Hussain, L., Asif, M., Mehmood, M. H., Imran, I., Anam Younas, Mahdy, A., Al-Joufi, F. A., & Abed, S. N. (2022). Polycystic Ovary Syndrome: A Disorder of Reproductive Age, Its Pathogenesis, and a Discussion on the Emerging Role of Herbal Remedies. In Frontiers in pharmacology (Vol. 13, pp. 874914–874914). Frontiers in pharmacology. https://doi.org/10.3389/fphar.2022.874914
[2] Hajam, Y. A., Rather, H. A., Neelam, Kumar, R., Basheer, M., & Reshi, M. S. (2024). A review on critical appraisal and pathogenesis of polycystic ovarian syndrome. In Endocrine and Metabolic Science (Vol. 14, p. 100162). Elsevier BV. https://doi.org/10.1016/j.endmts.2024.100162
[3] Khan, M. J., Ullah, A., & Basit, S. (2019). Genetic Basis of Polycystic Ovary Syndrome (PCOS): Current Perspectives. In The application of clinical genetics (Vol. 12, pp. 249–260). The application of clinical genetics. https://doi.org/10.2147/TACG.S200341
[4] Toosy, S., Sodi, R., & Pappachan, J. M. (2018). Lean polycystic ovary syndrome (PCOS): an evidence-based practical approach. In Journal of diabetes and metabolic disorders (Vol. 17, Issue 2, pp. 277–285). Journal of diabetes and metabolic disorders. https://doi.org/10.1007/s40200-018-0371-5
[5] Johnson, J.-E., Diandra Daley, Tarta, C., & Stanciu, P. I. (2023). Risk of endometrial cancer in patients with polycystic ovarian syndrome: A meta-analysis. In Oncology letters (Vol. 25, Issue 4, pp. 168–168). Oncology letters. https://doi.org/10.3892/ol.2023.13754
Being told you have an ovarian cyst often leaves you with more questions than […]
Chronic bloating. Lower back pain. Fatigue that lingers even after rest. These are symptoms […]
Many women live with Polycystic Ovary Syndrome (PCOS) without realising fact from fiction. This […]





Aster Gynaecology © | All Rights Reserved.