Being told you have an ovarian cyst often leaves you with more questions than […]

Have you been feeling discomfort in your lower abdomen, leaking a bit when you laugh or cough, or even struggling with a nagging sensation of pressure sensation “down below” that just won’t go away? These are symptoms which many women experience but often brush aside, thinking it’s just a normal part of ageing or life after childbirth. But what if it’s more than that?
Your pelvic floor is a powerful, yet often overlooked, set of muscles that play a crucial role in supporting your pelvic organs, which consist of your bladder, uterus and rectum. When functioning properly, these muscles help you control urination, bowel movements and even sexual function. However, when the pelvic floor is weakened or damaged, it can lead to a variety of issues that fall under the category of pelvic floor disorders or pelvic floor dysfunction (PFDs).
Despite being common, many women go years without realising they’re suffering from a pelvic floor disorder as the symptoms can be subtle, slow to develop, or mistaken for other conditions. In this article, we will highlight five key signs that you might have a pelvic floor disorder—so you can stop guessing and start seeking the right help.
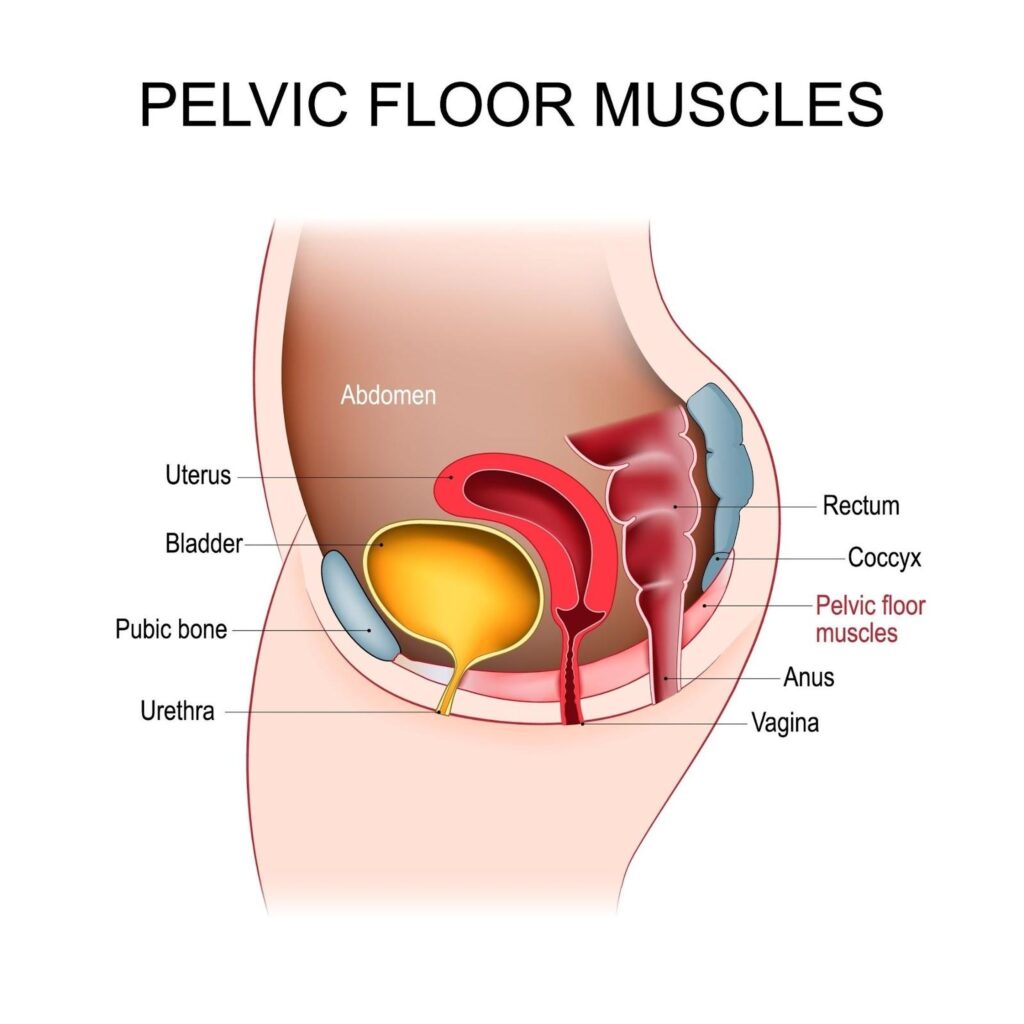
A pelvic floor disorder (PFD) occurs when the muscles and connective tissues in the pelvic area weaken, become overly tight or lose their ability to support the pelvic organs effectively. The pelvic floor is a complex network of muscles and ligaments that forms a hammock-like structure at the base of your pelvis. Its primary function is to support organs like the bladder, uterus and rectum and ensure they function properly. The pelvic floor muscles are also responsible for controlling bladder and bowel movements, as well as playing a key role in sexual function.
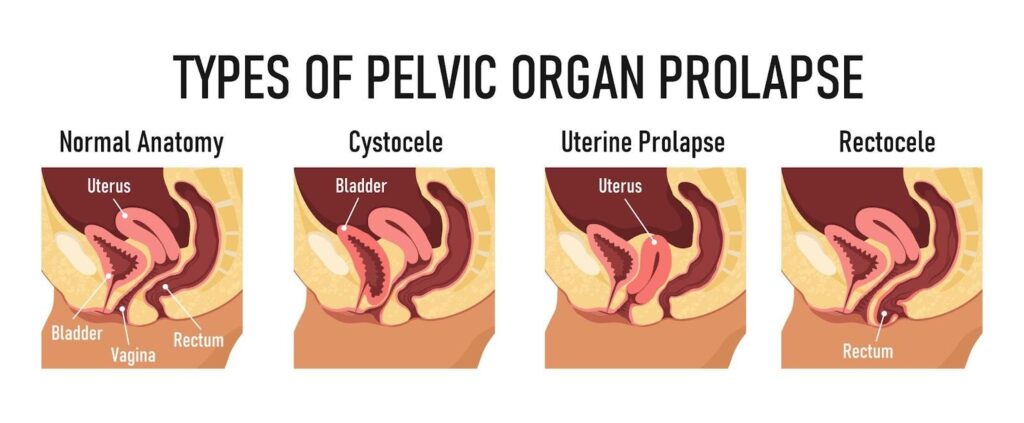
When these muscles are compromised—either through weakening, excessive strain or damage—they may not be able to perform their role efficiently leading to a pelvic floor disorder. This can result in issues like urinary incontinence, pelvic organ prolapse (when the organs drop and push against the vaginal walls) and chronic pain in the pelvic region.
Some of the most common causes of pelvic floor disorders include:
While it’s true that pelvic floor disorders are more commonly diagnosed in older women, they are not exclusive to this group. Women of all ages can experience pelvic floor issues, particularly those who have gone through childbirth, are overweight or engage in activities that put stress on the pelvic region. Young, active women can also suffer from pelvic floor disorders due to high-impact sports or improper lifting techniques.
Recognising the signs of a pelvic floor disorder (PFD) can help you seek treatment early and improve your quality of life. Here are five common symptoms that may indicate a problem with your pelvic floor:
One of the most common signs of pelvic floor dysfunction is urinary or bowel incontinence, particularly stress incontinence. This happens when the pelvic floor muscles fail to adequately support the bladder or rectum, leading to accidental leaks. You might notice this during simple activities like sneezing, coughing, laughing, jumping or exercising.
For many women, a little leakage here and there might seem harmless—perhaps you may be laughing with friends or lifting weights at the gym when it happens. However, even occasional leaks can indicate a weakened pelvic floor. While this may be brushed off as a “normal” part of ageing or post-childbirth life, it is a sign of stress incontinence and should not be ignored. Treatment options can significantly reduce/eliminate this symptom and prevent this from getting worse with time.

Another common symptom of a pelvic floor disorder is a persistent feeling of pressure or heaviness in the pelvic area. This can be a sign of pelvic organ prolapse, where one or more organs (bladder, uterus, or rectum) begin to slip out of place and push against the vaginal walls.
Women often describe this feeling as a sensation of “something falling out” or a heaviness that worsens after standing for long periods or towards the end of the day. This symptom is frequently ignored because it may come and go, but pelvic organ prolapse is a serious condition that can lead to further complications if left untreated. Early recognition can help prevent the need for surgical intervention.
If you experience pain during intercourse, known as dyspareunia, this could be another sign of pelvic floor dysfunction. Tight or overactive pelvic floor muscles can cause discomfort or pain during penetration, which makes sex unpleasant or even unbearable for some women.
The emotional toll of painful intercourse can be significant, leading to feelings of embarrassment, frustration or guilt. Over time, this may strain relationships or pose challenges in trying for pregnancy. Some women may feel ashamed to talk about it, fearing it’s an issue they have to live with. However, this is a common and treatable condition. Pelvic floor physiotherapy and other medical interventions can help alleviate the pain and restore a fulfilling sexual experience.
Another red flag for a pelvic floor disorder is difficulty in completely emptying the bladder or bowels. You may feel like you need to strain or push harder than usual to urinate or have a bowel movement, or experience a constant urge to go, even when your bladder or bowel is not full.
These issues can be frustrating and disruptive to daily life. Imagine being out at a social event, constantly feeling the need to visit the restroom, or experiencing the discomfort of never quite finishing a bowel movement. These symptoms not only affect physical health but also cause emotional stress. Treatment can address these issues and provide relief.
Pelvic floor dysfunction can also manifest as chronic lower back or abdominal pain, especially when other potential causes (like injury or muscle strain) have been ruled out. Because the pelvic floor muscles are interconnected with the muscles in your lower back and abdomen, any dysfunction can cause tension and discomfort in these areas.
Many women may not immediately associate their back or abdominal pain with pelvic floor issues, often assuming the pain is due to poor posture or normal muscle fatigue. However, chronic or unexplained pain in these regions may be a sign that your pelvic floor muscles are struggling to support your pelvic organs properly.
If you’re experiencing any of the signs mentioned earlier—whether it’s leaking urine during a laugh, feeling pressure in your pelvis, or dealing with lower back pain that you can’t quite explain—it’s essential to seek medical advice. While it may feel tempting to brush these symptoms aside as “just part of getting older” or something that will resolve on its own, these are often early indicators of pelvic floor dysfunction that can worsen over time if left untreated.
The good news is that pelvic floor disorders are highly treatable, especially when addressed early. Seeking help from a urogynaecologist can lead to effective treatment options, whether through pelvic floor therapy, lifestyle modifications, medications, or in more severe cases, surgical intervention. Early intervention not only helps manage the symptoms but can prevent further complications and help you regain control over your overall health and well-being.
Opening up about pelvic floor issues can feel awkward or uncomfortable, but it’s important to remember that your doctor is there to help, and these are common issues they address regularly. Here’s how you can begin the conversation with your urogynaecologist:
Once you’ve identified the signs of a pelvic floor disorder, the next step is exploring treatment options. The good news is that pelvic floor disorders (PFDs) are highly treatable and the range of available treatments can be tailored to your individual needs. From non-invasive therapies to more advanced surgical interventions, treatment plans are designed to address the specific symptoms you’re experiencing and the underlying causes of your pelvic floor dysfunction.
One of the most common and effective treatments for PFDs is pelvic floor physical therapy [6]. This specialised therapy focuses on strengthening or relaxing the pelvic floor muscles, depending on your condition. Although watching videos etc can sometimes be helpful, the connection between the brain and pelvic floor muscles can sometimes be difficult for women to establish reliably. A physical therapist trained in pelvic health will guide you through exercises like Kegels, which target the pelvic muscles and help improve control over bladder and bowel function. They may also use techniques such as biofeedback, electrical stimulation, or manual therapy to enhance muscle coordination and relieve pain.
Pelvic floor therapy is particularly effective for women with stress incontinence, pelvic organ prolapse, or dyspareunia (painful intercourse). It is a non-invasive option that can yield significant improvements with consistent practice and professional guidance.

For many women, making lifestyle changes can greatly improve pelvic floor health. Maintaining a healthy weight, for instance, reduces the strain on the pelvic muscles, especially in women who are overweight or obese. Adopting a fibre-rich diet can help manage constipation, which is a common cause of pelvic floor strain. Avoiding heavy lifting or learning proper techniques to minimise pressure on the pelvic muscles can also prevent further damage.
In addition to dietary and activity modifications, practising good posture and engaging in pelvic floor-friendly exercises (such as low-impact activities like walking, swimming or yoga) can help prevent symptoms from worsening.
In some cases, medications may be prescribed to manage symptoms of pelvic floor disorders. For instance, women with overactive bladder or urge incontinence may benefit from bladder relaxants that help reduce the urgency and frequency of urination [7]. Hormonal treatments, such as topical oestrogen, can also be useful, particularly for postmenopausal women whose symptoms are linked to hormonal changes affecting pelvic tissue strength and elasticity.
These medications can offer relief, but they are often used in combination with other treatments, such as pelvic floor therapy, to address the root cause of the dysfunction.
Vaginal pessaries can be particularly helpful for women who are experiencing bothersome pelvic organ prolapse – they are inserted into one’s vagina and act as mechanical support to alleviate symptoms of pelvic organ prolapse(without the need for surgery) and do not interfere with one’s daily routines. These come in many different shapes and sizes and fitting is done by a trained healthcare professional. Women can be taught how to self-manage and incorporate these to complement various activities/ exercises they may engage in as part of their lifestyle.
For women with more severe cases of pelvic organ prolapse or incontinence – surgery may be necessary. Surgical options vary based on the type and severity of the pelvic floor disorder. Common surgeries include sling procedures to support the bladder [8], colporrhaphy to repair weakened vaginal walls [9] or hysterectomy in extreme cases of uterine prolapse.
Surgery is typically reserved for when non-invasive treatments have not been effective. The decision to undergo surgery should be made after careful discussion with your healthcare provider. While surgery can offer a more permanent solution to severe PFDs, it’s important to weigh the risks and recovery time involved.
It’s important to remember that no two pelvic floor disorder cases are the same. The treatment that works for one woman may not be effective for another. This is why personalised care is crucial. Your gynaecologist will develop a treatment plan based on the specific symptoms you’re experiencing, your medical history and your lifestyle.
While pelvic floor disorders (PFDs) are common, there are several steps you can take to help prevent them or reduce the risk of worsening symptoms. Prevention starts with maintaining the health and strength of your pelvic floor muscles, along with making smart lifestyle choices that minimise strain on this crucial part of your body. Here are some practical and effective ways to protect your pelvic health:
One of the simplest yet most effective ways to prevent pelvic floor dysfunction is by incorporating Kegel exercises into your daily routine. Kegels specifically target the pelvic floor muscles, which helps in strengthening them and maintaining their ability to support your pelvic organs.
To perform a Kegel exercise, imagine you’re trying to stop the flow of urine midstream or trying to stop a fart from coming out. Squeeze and hold the muscles for a few seconds, then relax. Repeat this several times a day. The great thing about Kegels is that you can do them anywhere (except whilst on the toilet bowl to avoid confusing your bladder/rectum) —whether you are sitting at your desk or relaxing at home. Over time, consistent practice can reduce your risk of incontinence and pelvic organ prolapse.
By maintaining a healthy weight, you can reduce the strain on your pelvic muscles and improve overall pelvic health. This does not mean you need to aim for rapid weight loss. Instead, focus on sustainable lifestyle changes, such as eating a balanced diet rich in fruits, vegetables and whole grains, and engaging in regular physical activity. Managing your weight not only supports your pelvic floor but also contributes to your overall well-being.
Many women unknowingly strain their pelvic floor when lifting heavy objects, which can lead to dysfunction over time. To protect your pelvic floor, always use proper lifting techniques:
These simple adjustments can make a big difference in protecting your pelvic muscles from unnecessary strain.
Chronic constipation can be a significant contributor to pelvic floor disorders. To avoid this, focus on maintaining good bowel health by:
If constipation is a recurring issue, it’s important to address it early by consulting a relevant specialist and avoid prolonged straining, which can damage the pelvic floor over time.
Engaging in regular physical activity is essential for overall health, but not all exercises are pelvic floor-friendly. High-impact activities like running or heavy weightlifting can sometimes place excessive strain on the pelvic floor. Instead, focus on low-impact exercises that are gentle on your pelvic muscles while still keeping you active.
Swimming, walking and yoga are excellent examples of pelvic floor-friendly exercises that promote overall fitness without placing undue stress on the pelvic region. These activities can help you maintain strong muscles, reduce your risk of injury, and support your pelvic floor’s health.
By incorporating these preventive measures into your lifestyle, you can significantly reduce the risk of developing pelvic floor disorders. Preventing PFDs is all about staying mindful of how you use and care for your body—strengthening your muscles, avoiding unnecessary strain, and making smart choices that support your long-term pelvic health.
Recognising the early signs of a pelvic floor disorder is the first step toward regaining control of your health and well-being. By being aware of the symptoms and seeking medical advice early, you can address these issues before they progress. With proper treatment, whether through pelvic floor therapy, lifestyle changes, or other interventions, it’s entirely possible to manage and even resolve pelvic floor dysfunction.
Remember, you don’t have to live with discomfort, pain or embarrassment. With the right support and care, you can significantly improve your quality of life and enjoy a more active, comfortable, and fulfilling day-to-day routine.
If you’re experiencing any of the signs mentioned in this article, don’t hesitate to reach out. Contact our clinic today to schedule an evaluation and take the next step toward restoring your pelvic health. We are here to help answer your questions and guide you on your journey to wellness.
Being told you have an ovarian cyst often leaves you with more questions than […]
Chronic bloating. Lower back pain. Fatigue that lingers even after rest. These are symptoms […]
Many women live with Polycystic Ovary Syndrome (PCOS) without realising fact from fiction. This […]





Aster Gynaecology © | All Rights Reserved.