
Urinary incontinence (UI) is a common condition affecting millions of men and women worldwide, and occurs when one leaks urine involuntarily.
There are several types of urinary incontinence, namely:
1. Stress Urinary Incontinence (SUI): where one leaks urine involuntarily during physical activity i.e. on coughing, sneezing, jumping, laughing or exercising.
2.Urge urinary incontinence (UUI): when one leaks urine involuntarily shortly after experiencing a strong urge to urinate, i.e. not able to make it to the toilet in time after the feeling of needing to urinate hits you.
3. Mixed urinary incontinence (MUI): where one leaks urine involuntarily under both the fore-mentioned circumstances.
4. Overflow urinary incontinence: where one leaks or dribbles urine involuntarily (and without sensation) when the bladder is too full/overdistended.
What causes urinary incontinence in women?
The major causes of female urinary incontinence include:
Weakened pelvic floor muscles
A woman’s pelvic floor muscles form the base of the pelvis and work like a hammock to support the pelvic organs, which include the bladder, uterus (womb) and rectum. Risk factors that damage a woman’s pelvic floor includes;
- Damage sustained from pregnancy and childbirth
- Chronic stress on the pelvic floor muscles from obesity
- Chronic cough/constipation
- Lifting of heavy loads
- Ageing
- Menopause
Weakened bladder muscles
Aging results in degeneration and nerve damage, resulting in urinary incontinence.
Urinary Tract Infections (UTIs)
These can result in painful urination, foul-smelling urine, urinary frequency and urgency and UI as well. These symptoms typically resolve after treatment of UTI.
Other things that can worsen female urinary incontinence include:
- Drinking caffeine e.g. tea, coffee and alcohol
- Medical conditions such as poorly controlled asthma, chronic cough, suboptimal diabetic control
- Smoking
What causes urinary incontinence in men?

Majority of male urinary incontinence revolves around:
Prostate problems
As a man’s prostate gets enlarged, this leads to urinary symptoms such as frequent urination, weak stream and UI. In cases where the prostate is resected e.g. for cancer, SUI may occur as a result in men as well.
Nerve damage
Neurological conditions like Parkinson’s disease, stroke, diabetes, spinal cord disease, dementia can cause male UI. Surgery to the lower back or major bowel surgery can sometimes also cause nerve damage that manifests in UI.
Urinary Tract Infections (UTIs)
Similar to women, urinary tract infections can result in painful urination, foul-smelling urine, urinary frequency and urgency and urinary incontinence as well. These symptoms typically resolve after treatment of UTI.
Factors that aggravate urinary incontinence in women can also do the same for men.
Is urinary incontinence more common in women or men, and why?
The prevalence of UI in men is much lower than in women, about 3-11% overall, with UUI accounting for 40-80% of all male patients. SUI takes up less than 10%[1] of male cases and is usually due to prostate surgery, trauma or neurological injury.
Urinary incontinence remains a big problem in women - a local study[2] looking at 1119 healthy Singaporean mid-life women aged 45-69 years revealed that over 1 in 2 reported the presence of any UI, with MUI and SUI each affecting 20% of women – and these were statistics in women who were not actively seeking medical attention for their urinary incontinence, which tells you the dismal awareness of both patients and healthcare professionals about this major morbidity.
The main reason why the prevalence of urinary incontinence is so different between men and women is because our urinary tracts are built very differently in terms of anatomy, and women go through significant life events such as pregnancy and childbirth that men do not – it is hard being a woman indeed!
How does urinary incontinence differ between men and women?
In general, SUI is more commonly experienced by women as opposed to men due to damage sustained from pregnancy and childbirth; whilst if men are affected by urinary incontinence, it is more likely to be that of urge urinary incontinence.
Women are also much more prone to getting UTIs compared to men, as their urethra (urine pipe that transmits urine from the bladder to the urinary meatus i.e. external opening of the body) is considerably shorter due to the absence of penile length – a local study published in the Singapore Medical Journal[3] showed that adult women are 30 times more likely than men to develop UTI.
Conversely in men, the prostate can play a confounding role in the presentation of urinary symptoms in men, where enlargement can result in bladder outlet obstruction (BOO) - rare in women - and manifest in overactive bladder.
Once either gender starts experiencing symptoms of urinary incontinence, however, the severity and impact on one’s quality of life remains the same.
Someone suffering from urinary incontinence may face difficulty in maintaining perineal hygiene, find that their lives revolve around the (nearest) toilet, or feel embarrassment from the perennial “urine” smell emulating from down below with the potential need of wearing adult pads or diapers to avoid “accidents” – over time, this can have a significant impact on one’s ability to go about their daily lives normally, greatly reduce one’s self-esteem and body perception, and even adversely affect interpersonal relationships and sex life.
Are treatment options the same?
Treatment options of urinary incontinence depend more on the cause of incontinence rather than being gender specific, e.g. antibiotic treatment in cases of urinary tract infections (UTIs), or anticholinergic medications/behavioral therapy in cases of overactive bladder and/or UUI.
In cases of weakened pelvic floor muscles for example, the mainstay of treatment involves Kegels (pelvic floor) exercises, which can be taught bedside and reinforced with aid from a trained physiotherapist.
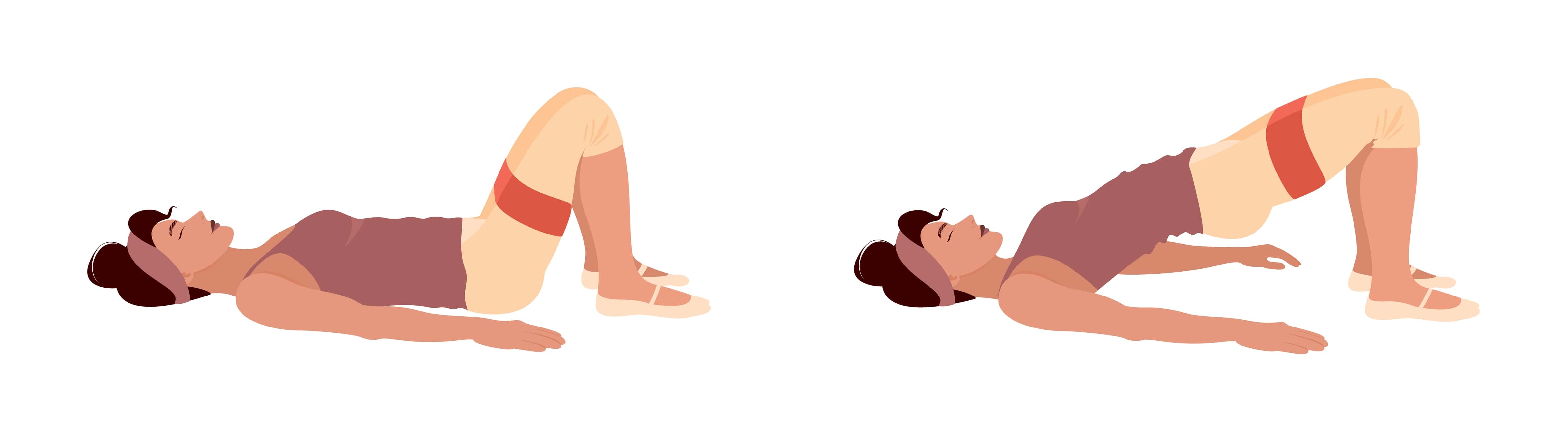
The aim and function of Kegels exercises are to strengthen the bulk and tone of one’s pelvic floor and alleviate the symptoms of SUI; to a certain extent, it can also help as part of bladder training for overactive bladder and UUI.
For female SUI that remain refractory to Kegels exercises, surgical intervention such as a mid-urethral sling or colposuspension may be considered.
Lifestyle modifications to reduce or avoid factors that aggravate the symptoms of urinary incontinence can be helpful in both genders - this includes;
- Reduction in caffeine/alcohol intake
- Smoking cessation
- Optimisation of body mass index via adoption of a healthy diet/exercise regimen
In cases where the prostate is contributory to urinary incontinence, a urologist’s input may be required to address this. Neurological disorders resulting in urinary incontinence can be complex to manage and a multi-disciplinary approach needs to be taken to optimize control of the relevant medical condition.
Conclusion
All in all, treatment options need to:
1. Be tailored to the individual
2. Target the predominant complaint/ symptoms that causes the most bother, i.e. if one suffers from MUI but experiences bothersome UUI more often than SUI, the stepwise approach is generally to target the symptoms of UUI first and foremost.
A simple and objective way that one can use at home to track one’s progress in the management of urinary incontinence would be via a bladder diary, which is a self-assessment tool that allows one to record how much and when they drink fluids, as well as how much and when they void, including episodes of urinary incontinence, if any.
An example of that can be found here, and will serve as a helpful adjunct to monitoring treatment for both the patient as well as the healthcare professional.
References
1. Nitti V. W. (2001). The prevalence of urinary incontinence. Reviews in urology, 3 Suppl 1(Suppl 1), S2–S6.
2. Ng, K. L., Ng, K., Thu, W., Kramer, M. S., Logan, S., & Yong, E. L. (2020). Risk factors and prevalence of urinary incontinence in mid-life Singaporean women: the Integrated Women's Health Program. International urogynecology journal, 31(9), 1829–1837. https://doi.org/10.1007/s00192-019-04132-3
3. http://www.smj.org.sg/article/urinary-tract-infections-adults