
Uterine fibroids are benign (non-cancerous) growths of the uterus that are commonly found in women of reproductive age.
A study published in the International Journal of Gynecology and Obstetrics[1] showed that fibroids, otherwise known as leiomyomas or myomas for short, are diagnosed in up to 70% of white women and over 80% of African ancestry women during their lifetime. 30% of women with fibroids will present with severe symptoms requiring intervention.
Uterine fibroids appear to contain genes differing from the usual uterine muscle cells, and their growth is typically promoted by estrogen and progesterone, the 2 female hormones in a woman’s body. Several risk factors may put one at higher risk of uterine fibroids, including:
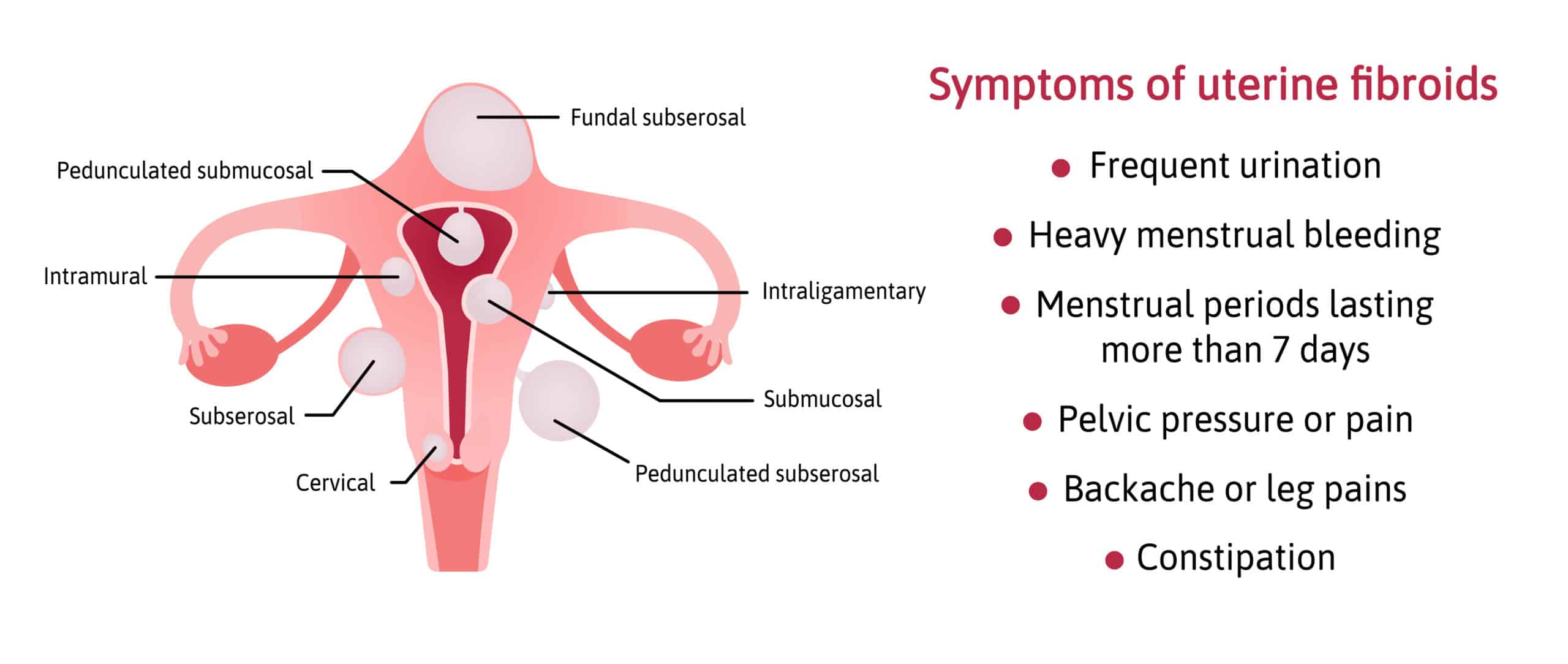
Fibroids are classified according to their location, namely:
These are the ones located on the outer layer (serosa) of the uterus, and typically do not require treatment until they become symptomatic.
These arise predominantly within the uterine muscle wall layer (myometrium) and can be symptomatic
These grow towards the inner layer (mucosa) of the uterus and bulge into the uterine cavity. Small submucous fibroids can already cause significant symptoms due to their unique location, and also tend to have the largest impact on fertility and pregnancy.
Uterine fibroids are largely non-cancerous; studies have shown the risk of malignant transformation of fibroids is less than 0.5.%.
Despite this, they do have the potential to cause significant symptoms, although many women are lucky enough to be asymptomatic from their fibroids and may only be incidentally picked up during a health screening.
Symptoms are influenced by the size, location and number of uterine fibroids and can include:
Most uterine fibroids exhibit slow growth over the years although not every fibroid behaves the same way - with some staying the same size for years and others growing rapidly over a short period of time.
As fibroid growth is promoted by estrogen and progesterone, the growth of uterine fibroids typically stops once a woman attains menopause (which corresponds to a drop in the level of female hormones in the body) and will usually shrink from there on. Small fibroids may disappear as a woman spends more years in menopause, but sizable fibroids at the onset of menopause may still remain albeit at a smaller size.
The pain that uterine fibroids cause is typically related to the heavy menstrual flow that they cause - many women describe their menstrual pains to coincide with the passage of blood clots during their periods.
In less common cases, fibroids can cause pain during pregnancy (red generation, as mentioned above) or during the non-pregnant state if the fibroid happens to be pedunculated and undergoes torsion (i.e. twisting around its pedicle and causing cut-off of the blood supply).
In general, if your uterine fibroids are not causing you any symptoms or problems, you can opt to leave them alone and check in with your gynaecologist on a regular basis to monitor your fibroid(s) via pelvic ultrasound.
Treatment is individualised and will depend on your age, the severity of symptoms you are experiencing, the size/location/number of uterine fibroids, and your fertility intention. Some management options for uterine fibroids include:
| Treatment | How it works |
| Non-hormonal medications | These include non-steroidal anti-inflammatory drugs (NSAIDs) and oral tranexamic acid, which are taken on an as-needed basis during the period and serve to reduce menstrual cramps and period flow. Non-hormonal medications do not shrink the fibroids nor prevent fibroid growth. |
| Hormonal medications | These include progesterones or birth control pills, which serve to reduce menstrual flow and can help to regulate one’s periods and/or provide contraceptive cover if required.
Hormonal medications also do not shrink the fibroids nor prevent fibroid growth. In recent years, the Food Drug Administration (FDA) have approved newer hormone-based medications (Oriahnn and Myfembree) to manage heavy menstrual bleeding caused by fibroids; usage of these are not yet mainstream due to the risks of bone loss with treatment period limitation of 24 months. |
| Levonorgestrel-releasing intrauterine contraceptive device i.e. Mirena | Suitable for women with heavy menstrual bleeding from uterine fibroids who do not have distortion of their uterine cavity, Mirena can help reduce menstrual flow significantly, lasts for 5 years and also provides contraception. |
| Gonadotropin releasing hormone agonist (GnRHa) i.e. Lucrin | This is typically reserved for short-term, pre-operative shrinkage of uterine fibroids and is not usually used beyond a 6 month period due to side effects. |
| Transcervical hysteroscopic resection of fibroid | Performed through introduction of a scope into the uterine cavity from the vagina and is suitable only for submucous fibroids. |
| Myomectomy | Surgical procedure that can be done either laparoscopically or via the traditional open method (laparotomy) to remove fibroids and conserve the uterus in women still desiring fertility and/or not wanting to remove their uterus. There is a risk of fibroid recurrence. |
| Hysterectomy | Surgical procedure that can be done either laparoscopically or via the traditional open method (laparotomy) to remove the uterus.
The ovaries can be conserved depending on whether there is pathology and also depending on the woman’s age and wishes. A hysterectomy is suitable only for women who have completed their family or have no fertility desires, as after this operation one will have no more periods and will not have the ability to carry a pregnancy. |
Non-surgical methods to manage fibroids include;
It is important to note that not every woman with uterine fibroids is suitable for HIFU or UAE, as your age, fibroid location, number and size are factors that need to be taken into consideration before such procedures are embarked upon.
It is also paramount to understand that although fibroid shrinkage can be attained with these procedures, complete elimination of fibroids is typically not possible using these methods, hence the propensity for regrowth and recurrence with the potential of needing more procedures in future.
The UK National Institute for Health and Care Excellence (NICE)[2] guidelines on ultrasound-guided high-intensity transcutaneous focused ultrasound for symptomatic uterine fibroids states that the efficacy of HIFU in the treatment of uterine fibroids is limited in quality and should only be performed:
In addition, they also advised that clinicians tell patients that:
In a similar vein, the NICE[3] guidance on Uterine artery embolism for fibroids, while acknowledging that UAE is efficacious for symptom relief in the short and medium term for a substantial proportion of patients, cautioned that clinicians counsel their patients the same way as HIFU i.e. incomplete symptoms relief, the need for future procedures and the uncertainty of UAE effect on fertility and pregnancy.
If you have any questions, feel free to drop me a message and I’ll be happy to help!