Most women experience irregular periods at the start and towards the end of their reproductive lifespan; some women continue to have irregular periods throughout the majority of their menstruating lives.
But what constitutes the definition of irregular periods? The interval between periods should be counted from the first day of one period to the first day of the next period to ensure consistency.
Contrary to what most people think, a regular period does not necessarily have to be 28 or 30 days apart.
In this article, we’ll discuss:
- What an irregular period is
- When to worry about irregular periods
- Why irregular periods can be an indicator of PCOS
- Why it’s important to get treated for PCOS
What is considered an irregular period?
A normal interval between periods can be anywhere from 21 to 35 days - it varies between each individual woman and the most important thing is to know what is normal for yourself.
When should I be worried about irregular periods?
If you have a background of regular periods and have just encountered one episode of irregular periods i.e. your period suddenly came too early or too late, ensure that it is not pregnancy-related; if it is not, there is generally no need to panic and rush to your gynaecologist’s office.
It is worthwhile to:
- Observe for a few cycles
- Keep a menstrual calendar or diary (you can easily download an app to help you keep track), and see if this problem persists for more than a few months
- If it does, or if you encounter other period problems such as painful or heavy periods, unscheduled bleeding i.e. bleeding in between your periods (intermenstrual bleeding) or after sexual intercourse (post-coital bleeding), then see your gynaecologist for further checks
What is PCOS?
PCOS is short form for polycystic ovary syndrome, which is a common gynaecological condition afflicting many women of reproductive age. The Centers for Disease Control and Prevention (CDC) estimates that 6-12%[1] or as many as 5 million US women of reproductive age have PCOS, which is one of the most common causes of female infertility.
PCOS is diagnosed based on the Rotterdam[2] criteria, where one needs to fulfil at least 2 out of 3 diagnostic criteria:
- Oligo- or anovulation: Absence of ovulation is characterised by irregular or absent periods)
- Polycystic ovaries: Ovaries look larger than normal with increased number of follicles on scan; 12 or more follicles in each ovary measuring 2-9mm in diameter, and/or increased volume of >10ml)
- Clinical and/or biochemical signs of hyperandrogenism: Excessive presence of the male sex hormones in women that can either manifest physically or be diagnosed on blood test results
Note: Having one of the above does not necessarily mean that you have PCOS.
You need 2 out of 3 criteria at least; you will generally need to see a gynaecologist who will be able to take a detailed medical history, perform a physical examination as well as investigations such as pelvic ultrasound and blood tests to determine the likelihood of you having PCOS.
Although the exact cause of PCOS remains unknown, there seems to be a genetic predisposition to it. For example, if your mother had a history of PCOS, you may be at increased risk of having PCOS yourself.
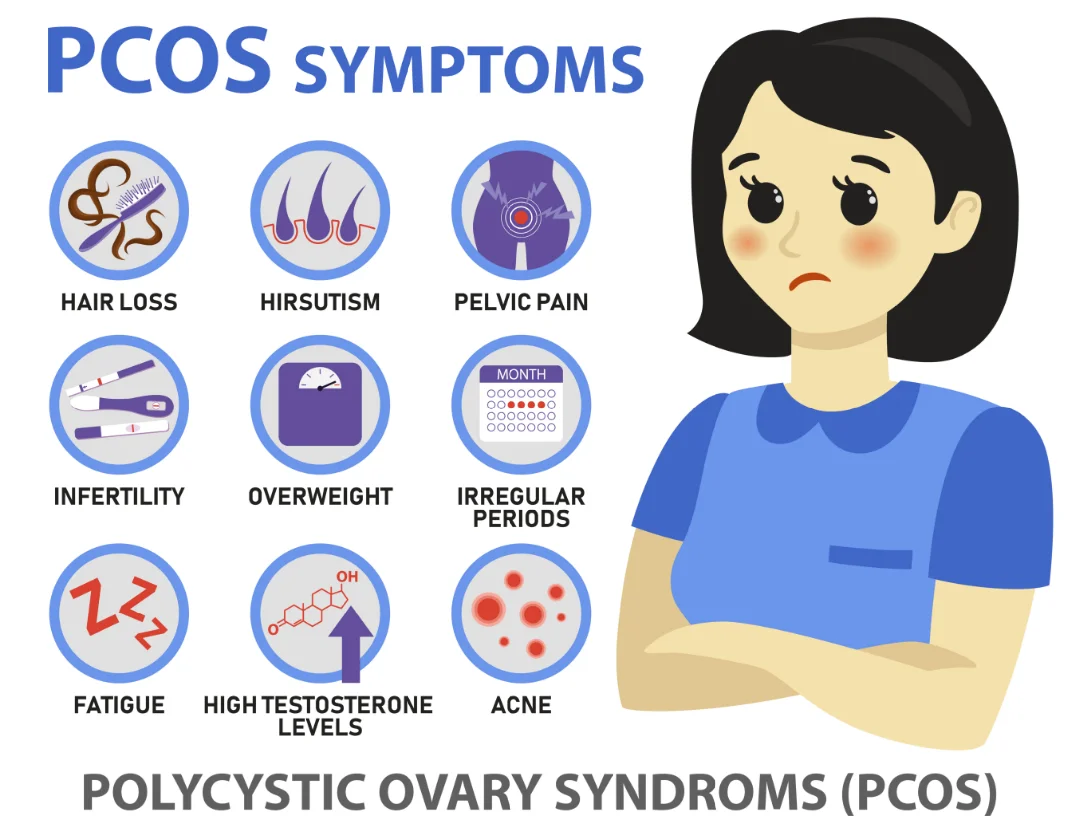
What are the symptoms of PCOS?
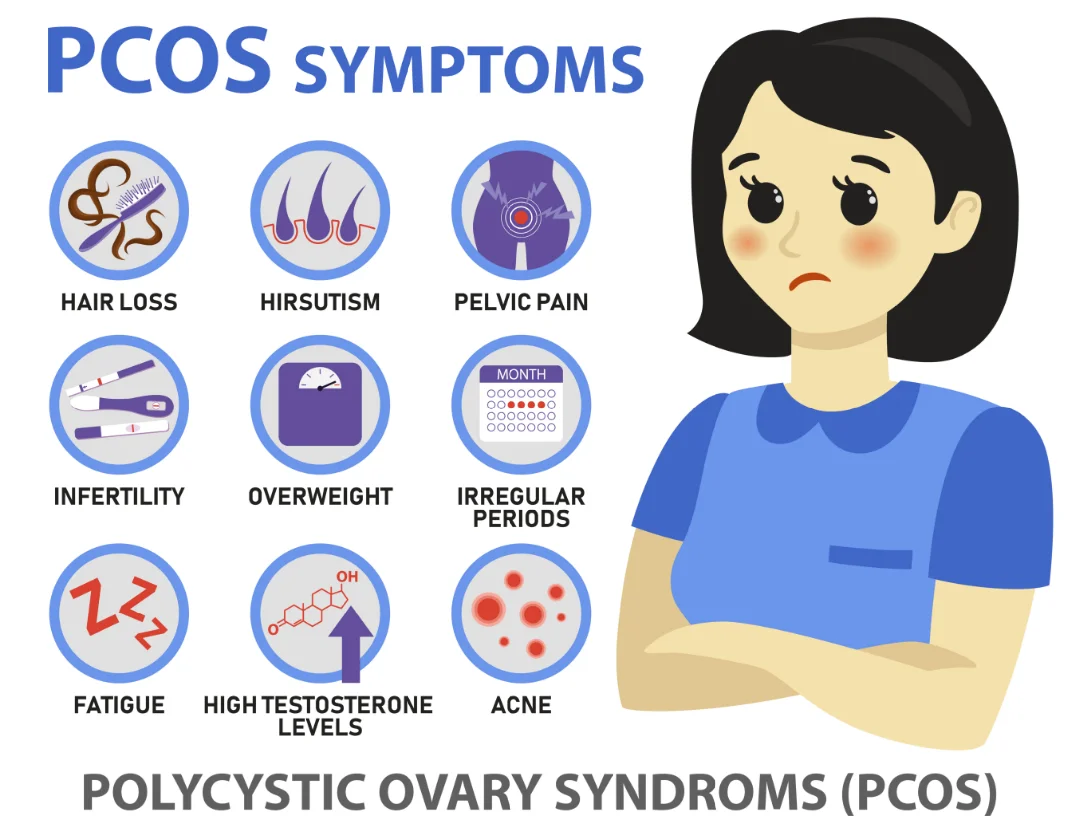
Not every woman with PCOS will manifest with symptoms. Symptoms of PCOS include:
- Irregular periods
Most women turn up at their gynaecologist’s office when they find themselves still having irregular or absent periods even after emerging from their teenage years; some women experience a period of regular menstrual cycles before going into irregularity.
- Infertility
The other common scenario would be presentation after trying unsuccessfully to conceive with their partner for several years i.e. infertility.
- Acne, excessive hair growth (hirsutism), ahir loss, darkening of the skin on body creases
e.g. on the back of the neck (acanthosis nigricans). These are signs of excessive male hormones in the body.
- Weight gain that is difficult to control
Women with PCOS tend to face issues with weight gain, high body mass index (BMI), with a link to insulin resistance.
As such, women with PCOS can be at an increased risk of developing other health problems such as:
- Gestational diabetes mellitus (GDM)
This is typically diagnosed based on a oral glucose tolerance test (OGTT) performed during weeks 24 to 28 of pregnancy and is a condition that can lead to increased pregnancy complications for both mother and child if poorly controlled.
- Diabetes mellitus (DM)
It is estimated that more than half of women with PCOS will develop DM by the age of 40 years old.
- Hyperlipidemia, or high cholesterol
Associated with elevated levels of LDL (bad cholesterol) and low HDL (good cholesterol).
- Hypertension
This, together with the fore-mentioned risk factors of DM and hyperlipidemia, leads to a higher risk of developing heart disease and stroke.
- Sleep apnea
This is a condition where one stops breathing temporarily during sleep.
- Emotional disturbances
Women with PCOS may have issues with mental health including depression, reduced self-esteem and/or anxiety.
- Endometrial cancer
Women with PCOS are at increased risk of developing cancer of the uterine (womb) lining especially if they have fewer than 3 periods a year; this is because the lining is continually thickened.
Why women with PCOS have irregular periods
Although some women with PCOS continue to have regular periods every month, women with PCOS tend to have irregular periods due to hormonal imbalances in their body.
High levels of androgens and insulin resistance disrupt the process of ovulation, where a mature egg is released from the ovary every month. This in turn disrupts the physiological cycle of menstruation, resulting in irregular periods or even absent periods.
It is not uncommon for women with PCOS to either have periods only once every few months, or not at all unless they take medications from the doctor’s office to induce their periods.
Can PCOS be cured?
As PCOS has important implications on your fertility and can put you at a greater risk of developing long-term health problems highlighted above, it is essential to seek help and obtain an early diagnosis if you suspect you may be having PCOS.
Treatment for PCOS include the following:
- Having a healthy lifestyle
This includes eating a balanced diet (meals at regular intervals) consisting of lean meats, fruits, vegetables, whole-grain foods and avoiding excessive amounts of sugar, salt, caffeine, alcohol and processed foods.
Try engaging in regular exercise of at least moderate intensity, 30 minutes three times a week (or more if you can afford the time). Seeking help from a dietician and/or physical trainer can help individualize your meal plan and exercise regime for better consistency.
- Going for regular health checks
To screen for the fore-mentioned conditions.
- Medications to induce your period (if you are having 3 or less periods a year)
This typically involves either progesterone tablets or combined birth control pills (depending on your needs), and will serve to reduce your risk of developing endometrial cancer in the future.
- Ovulation induction medications, or assisted reproductive techniques
For women with PCOS facing infertility issues and desiring pregnancy.
Do you have any questions for me? Feel free to contact me and I’ll reply as soon as I can.
References
- https://www.cdc.gov/diabetes/basics/pcos.html#:~:text=PCOS%20is%20one%20of%20the,beyond%20the%20child%2Dbearing%20years
- Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group (2004). Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Human reproduction (Oxford, England), 19(1), 41–47. https://doi.org/10.1093/humrep/deh098