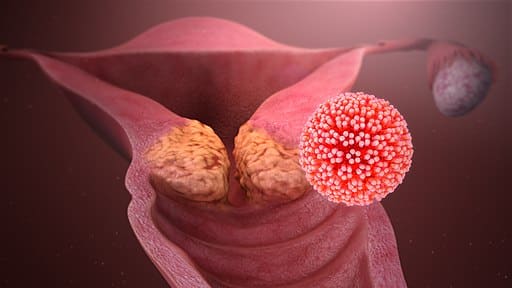
Cervical cancer is cancer arising from the neck of the womb.
The top reason for cervical cancer is persistent high risk human papillomavirus (HPV) infection. Read more about HPV in cervical cancer screening and how to prevent infection through a HPV vaccine.
The most common symptom is abnormal bleeding or vaginal discharge. Some women can have no symptoms at all, especially in the early stages. Symptoms can include:
Your gynaecologist will need to take a detailed medical history and perform a pelvic examination for you. Depending on the appearance of your cervix, you may need a Pap smear/HPV test, colposcopy and/or biopsy. A colposcope magnifies your cervix to better identify areas of abnormalities for biopsy – this can usually be done in the clinic.
Staging of the cancer is next. You will be asked to go for further imaging e.g. CT or MRI scans to check if the cancer is confined to your cervix or has spread beyond. In general –
Stage 1: cancer is in the cervix only
Stage 2: cancer has spread beyond the cervix and uterus, but has not spread to the pelvic walls or lower part of vagina
Stage 3: cancer has spread to the pelvic walls or lower part of vagina, with possible lymph node involvement
Stage 4: cancer has spread outside of the pelvis e.g. to the bladder, rectum, lungs etc
This depends on your age, general health, medical conditions and stage of cancer. Treatment can involve surgery, chemotherapy and/or radiotherapy. Your gynae-oncologist will be able to discuss with you about the options suitable for you.
Surgery usually involves total hysterectomy (removal of the uterus and cervix) and/or possible lymphadenectomy (removal of lymph nodes in the pelvis and abdomen to check for cancer involvement).
For chemo- and radio-therapy, your gynae-oncologist will manage you together with a medical oncologist to optimise your treatment.
Photo credit: www.scientificanimations.com / Wikimedia Commons