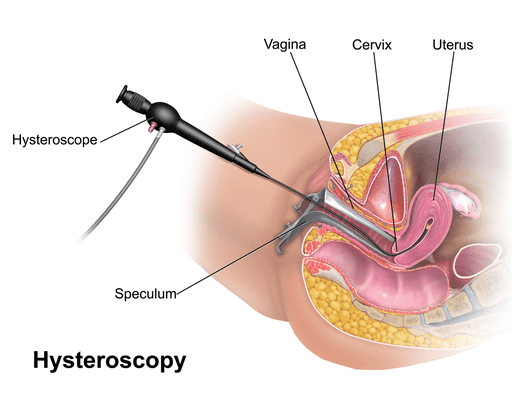
What is a hysteroscopy?
A hysteroscopy involves the insertion of a telescope camera through the cervix (neck of womb) into the uterus, with fluid instilled inside the uterus to open up the uterine cavity. This allows diagnosis (and in some cases, treatment) of abnormalities of the uterine cavity and lining.
Hysteroscopy is frequently performed to achieve a diagnosis when the following gynaecological conditions are suspected:
Hysteroscopy can also be used to treat some of the above conditions when combined with other procedures such as polypectomy (removal of endometrial polyps), excision of fibroids/septum, division of scar tissue, dilation and curettage etc.
Hysteroscopy is generally a safe and commonly done procedure.
Risks of hysteroscopy include:
Common risks:
Uncommon but potential serious risks:
Photo credit: BruceBlaus / Wikimedia Commons