Being told you have an ovarian cyst often leaves you with more questions than […]
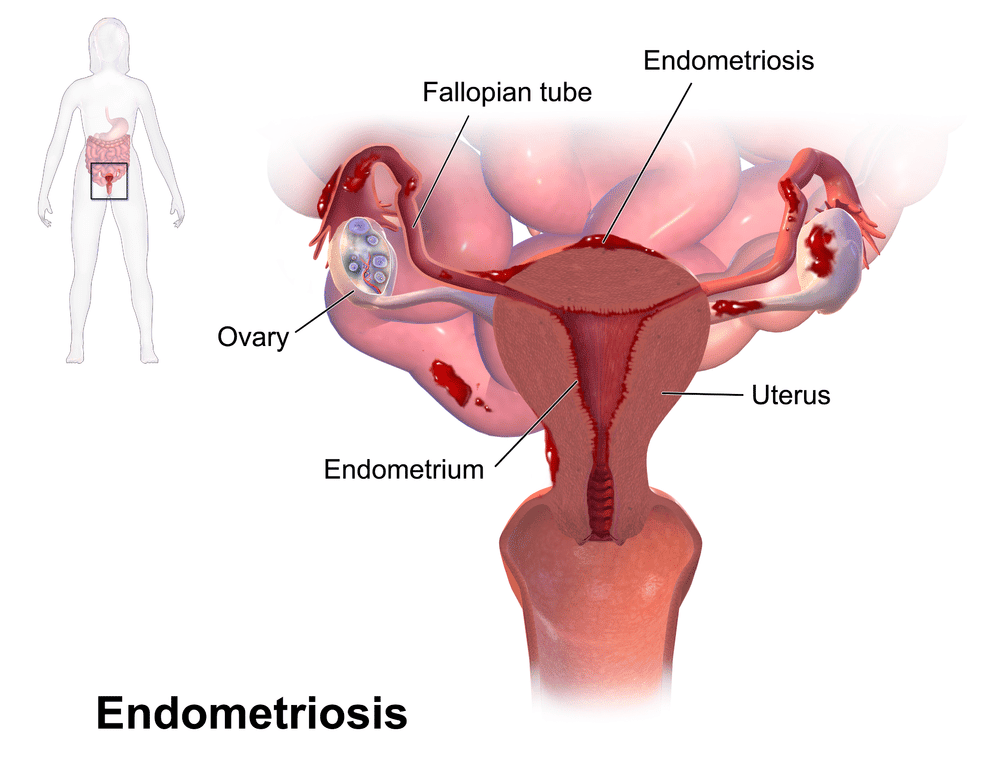
This article focuses on surgical treatment of endometriosis. Click here to find out about what endometriosis is, its symptoms and diagnosis.
This depends on how severe your symptoms are, the stage of endometriosis, and your fertility plans. Endometriosis is a long-term condition. There is no cure and multiple surgeries are not recommended.. The aim of treatment is to achieve surgical clearance at the most appropriate time, with hormonal medicines before and after that to suppress endometriosis.
Surgery is usually recommended for cases of advanced endometriosis with severe symptoms, or for women who wish to conceive soon but have difficulty getting pregnant. Depending on severity, a pre-operative MRI and a colorectal surgeon may need to be involved with your surgery.
Laparoscopy (keyhole) surgery under general anaesthesia allows for removal of endometriosis – this usually involves a 1cm cut in your umbilicus and three to four 0.5cm cuts in your abdomen. A laparoscope (camera) is inserted through your umbilicus and the extent of endometriosis determined. If there are endometriotic or “chocolate”/”blood” cysts in your ovaries, these will be removed (ovarian cystectomy). Endometriotic deposits in your pelvis will also be excised. Rarely, in severe cases where there is deep infiltrating endometriosis, the colorectal surgeon may need to perform shaving of endometriosis from the bowel or bowel resection (removing the section of bowel that has been affected by endometriosis).
If you are planning for pregnancy, additional procedures such as hysteroscopy to check your uterine cavity, hydrotubation (a dye test to check patency of your fallopian tubes) and ovariopexy (fixing your ovaries low down in the pelvis for better access during egg collection for in-vitro fertilisation) may be recommended.
Laparoscopic surgery for endometriosis is technically challenging due to long-term inflammation and scarring that the condition has caused – this usually results in adhesions between the intestines and pelvic organs. Anti-adhesion barriers (special bio-compatible materials) are typically placed at the end of the surgery to reduce the risk of adhesion reforming. In some cases, a laparoscopic procedure may need to be converted to a laparotomy (open) surgery. You will need to be hospitalised after the operation as it is a major surgery. Do discuss with your doctor who will be able to advise you on the risks of surgery in your specific case, and what to expect.
Hormonal medications to suppress endometriosis will need to be taken long-term, even if surgery has been done to clear endometriosis, unless you are trying to get pregnant, are pregnant or have reached menopause.
Photo credit: BruceBlaus / Wikimedia Commons
Being told you have an ovarian cyst often leaves you with more questions than […]
Chronic bloating. Lower back pain. Fatigue that lingers even after rest. These are symptoms […]
Many women live with Polycystic Ovary Syndrome (PCOS) without realising fact from fiction. This […]





Aster Gynaecology © | All Rights Reserved.