
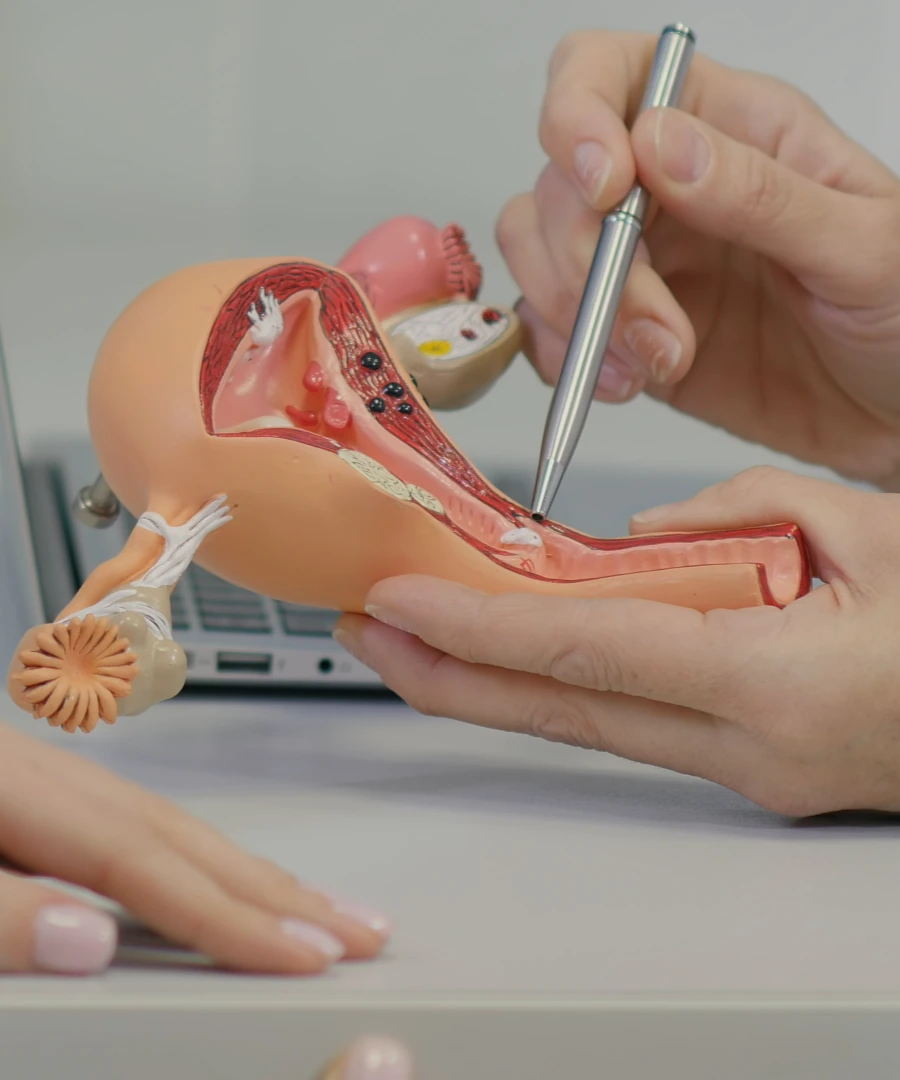
Gynaecological cancer is an umbrella term used in Singapore for the various types of cancer that can occur within or on a woman's reproductive genitals and organs.
The 6 main types of gynecologic cancer are:
Some of the most common gynaecological cancers in Singapore include:
Almost all cervical cancers are caused by HPV (human papillomavirus), which is a common sexually-transmitted viral infection that usually clears on its own.
While low-risk HPV can cause genital warts, it does not cause not cancer. High-risk HPV, however, can cause pre-cancerous changes which may develop into cervical cancer without intervention.
As HPV can be symptomless, it is therefore crucial to have regular cervical cancer screenings even if you’ve completed your HPV vaccinations. Generally, you should get screened every 3 years with a Pap test, and every 5 years with an HPV test.
Treatment options largely depend on your age, general health, reproductive wishes, medical conditions and stage of cancer. Treatment can involve surgery, chemotherapy and/or radiotherapy.
Surgery usually involves the following:
The HPV vaccine can prevent cervical cancer by offering protection against certain strains of HPV. In fact, HPV vaccination has been shown to protect against 70 to 90% of cervical cancers if given before the onset of sexual activity (depending on the vaccine type).
Although HPV vaccines cannot treat current infections, it can still offer some protection for those who are sexually active or already exposed to HPV. Currently, these are the recommended dosages for those aged 9 to 26:
As a universally safe vaccine with minimal side effects, the HPV vaccine usually only presents with mild, self-resolving side effects such as pain, slight swelling and/or redness at the injection site, and a temporary headache.
The most common symptoms are abnormal bleeding or vaginal discharge. However, do note that some women can be symptomless, especially in the early stages.
Symptoms of gynaecological cancer can include:

Cervical cancer ranks as the 11th most frequent cancer among Singaporean women, and is the 5th most common cancer among women aged 15 to 44. Here are the risk factors for the most common types of gynaecological cancers in Singapore:
A HPV test is performed similarly to a pap smear. A brush is used to lightly brush the cervix for a sample that is analysed for the presence of high-risk HPV. Because the HPV test is more sensitive than the traditional Pap smear, the screening interval for a negative test result is 5 years (instead of the traditional 3 years).
While HPV primary testing is recommended for women 30 years and above, women aged 25 to 29 should continue with routine pap smears, as HPV testing for this age group has a high incidence of temporary HPV infection.

One of the other ways that gynaecological cancer is diagnosed is by monitoring a patient’s Ca125 levels, as a rising Ca125 level may indicate a return or continued growth of cancer. Monitoring Ca125 levels is also useful in ovarian cancer management and treatment.
However, a high Ca125 level alone is not sufficient to diagnose gynaecological cancer, as a number of non-cancerous conditions (eg. UTI, pregnancy, endometriosis, liver disease etc.) can also cause a spike in Ca125 levels. Additionally, some women with ovarian cancer never develop high Ca125 levels.
In order to properly diagnose gynaecological cancer, your doctor will need to take detailed notes of your medical history, perform physical examination(s) such as a colonoscopy or biopsy, conduct ultrasound(s), and perform other necessary tests.
Once a biopsy has confirmed the presence of gynaecological cancer, your doctor will have you go for further imaging (eg. CT and MRI scans) to determine the stage of your cancer, ie. how far it has spread.





Aster Gynaecology © | All Rights Reserved.