Ovarian cancer is cancer arising from one or both of your ovaries. The majority of ovarian cancer arise in older women. 9 out of 10 cases are epithelial ovarian cancer, which is a cancer that develops from the cells surrounding the outer layer of the ovary.
In many cases, the exact cause is not known. Some risk factors may include:
Unfortunately, many women do not have symptoms until ovarian cancer is late stage. Symptoms are usually vague and may include:
Your gynaecologist will need to take a detailed medical history and perform a pelvic examination for you. A transvaginal ultrasound will be done to check your uterus and ovaries. Blood tests (tumour markers e.g. Ca125) may be advised. Depending on your ultrasound and blood test results, you may be asked to go for further imaging e.g. CT scan. If there is fluid in your abdomen, some may be drained for testing. Another way to look into your abdomen directly is laparoscopy (keyhole) surgery, where biopsies can also be taken.
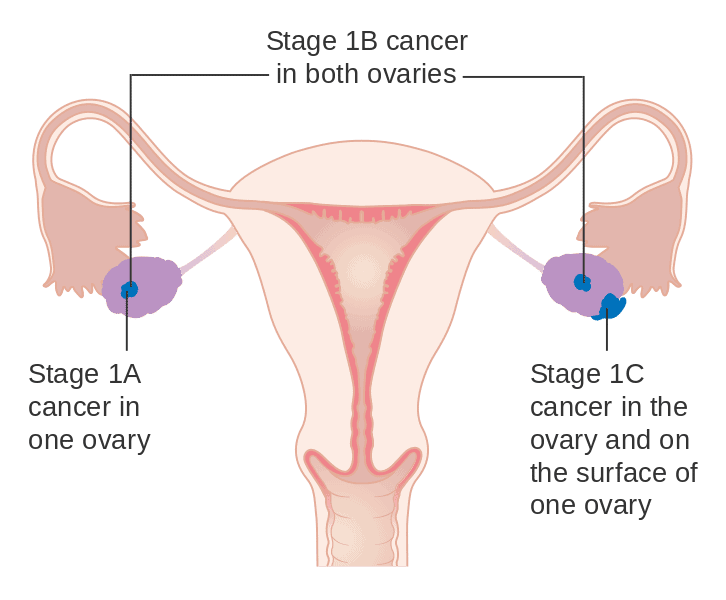
Staging of the cancer is next. In some cases, this can only be confirmed after surgery is done. In general –
Stage 1: cancer is in the ovary/ovaries only
Stage 2: cancer has spread beyond the ovaries, but has not spread beyond the pelvis
Stage 3: cancer has spread beyond the pelvis, but not involved other parts of the body
Stage 4: cancer has spread to other parts of the body e.g. to the liver, lungs etc
This depends on your age, general health, medical conditions and stage of cancer. Treatment can involve surgery, chemotherapy and/or radiotherapy. Your gynae-oncologist will be able to discuss with you about the options suitable for you.
Surgery usually involves hysterectomy (removal of the uterus), bilateral salpingo-oophorectomy (removal of both fallopian tubes and ovaries) and/or possible lymphadenectomy (removal of lymph nodes in the pelvis and abdomen to check for cancer involvement), omentectomy (removal of fat pad in the abdomen) and removal of appendix in some cases.
For chemo- and radio-therapy, your gynae-oncologist will manage you together with a medical oncologist to optimise your treatment.
Photo Credit: Cancer Research UK / Wikimedia Commons