What is endometrial hyperplasia?
This is a condition where the lining of the uterus becomes too thick. Although it is not cancer, it can progress to cancer of the uterus in some cases if left untreated.
What causes endometrial hyperplasia?
The lining of the uterus responds to female hormones. Estrogen is involved in the first half of the cycle, where the lining grows and thickens. After an egg is released (ovulation), progesterone comes in to prepare the lining of the uterus for pregnancy. If fertilisation does not occur, the lining is shed and a new cycle begins.
Endometrial hyperplasia occurs when there is excess estrogen without progesterone. This happens when ovulation does not occur and progesterone does not come in. The lining of the uterus continues to grow, the cells of the lining start to crowd together and there is no shedding. If this continues, it may eventually lead to cancer.
What are the symptoms of endometrial hyperplasia?
Abnormal bleeding is usually the first sign of endometrial hyperplasia. These include:
- heavy periods
- long periods
- bleeding in between periods
- bleeding after menopause
What are the risk factors for endometrial hyperplasia?
- Older age
- Having more periods in one’s lifetime (early age of first period and late age of last period i.e. menopause)
- No pregnancy before
- Obesity
- Certain medical conditions e.g. polycystic ovary syndrome (PCOS), diabetes
- Smoking
- Personal history of breast cancer and taking tamoxifen
- Family history of cancer of the uterus, ovary or colon
What are the types of endometrial hyperplasia?
Your gynaecologist will advise you on the type of endometrial hyperplasia you have, including:
- Hyperplasia without atypia: this has up to 5% risk of progressing to cancer with time if untreated
- Hyperplasia with atypia: this has up to 30% risk of progressing to cancer with time if untreated
Atypia increases the risk of progressing to cancer.
How will my gynaecologist diagnose endometrial hyperplasia?
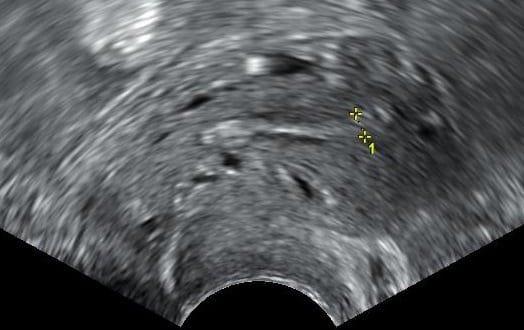
A transvaginal pelvic ultrasound scan is useful to measure thickness of the lining of the uterus; however, the only way to confirm would be through a biopsy of the uterus lining. This is either done in the clinic (endometrial pipelle), or as a day surgery under general anaesthesia (hysteroscopy dilation and curettage (D&C)). The biopsy will need to be examined under a microscope to diagnose endometrial hyperplasia, and whether atypia is present.
What is the treatment for endometrial hyperplasia?
This depends on your age, medical conditions, fertility plans, type of hyperplasia and willingness for long-term follow-up. Options include:
- Progesterone: This can come in the form of daily oral tablets or Mirena intrauterine device (IUD). The duration of treatment depends on the type of hyperplasia and your response to treatment, which will be determined by repeat biopsies of the uterus lining. Long-term follow-up is required because there is a risk of recurrence.
- Hysterectomy: this is an option for women not wanting future pregnancies or not able to come for long-term follow-up.
How can I reduce the risk of getting endometrial hyperplasia?
- Do not allow yourself to go for more than 3 months without periods – see your gynaecologist if this happens as you will need checks for conditions like PCOS, and hormone medications to induce your periods.
- Lead a healthy lifestyle to avoid obesity
- If you are taking hormone replacement therapy (HRT) and you have not had a hysterectomy before, you will need to take progesterone with estrogen.
Photo Credit: Mikael Häggström / Wikimedia Commons